After a craniotomy or a blow to the head, most patients focus on pain control, mobility and infection prevention. What often gets overlooked is the sudden surge of urinary issues-frequent trips to the bathroom, sudden leaks, or the inability to empty the bladder at all. Ignoring these signs can turn a recoverable problem into a long‑term disability.
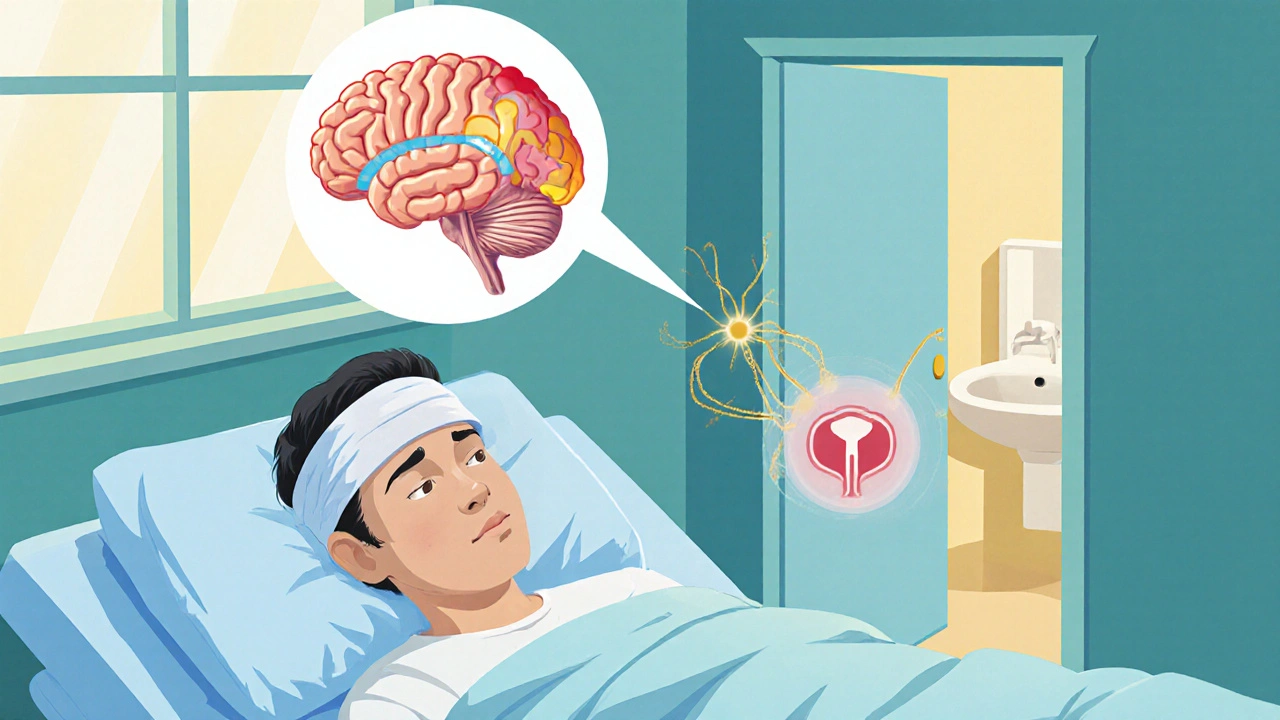
How the Brain Controls the Bladder
Bladder function is a team effort between the spinal cord, peripheral nerves and several brain regions. The Neurogenic bladder is a condition where nerve damage disrupts the normal signaling that tells the bladder when to fill and when to empty. The prefrontal cortex, pontine micturition center, and basal ganglia coordinate the desire to void with the muscles that hold urine in. Damage to any of these areas-common after a traumatic brain injury is a disruption of brain tissue caused by a violent impact, such as a fall or vehicle collision-throws the system off balance.
Typical Urinary Problems After Head Injury or Surgery
- Overactive bladder (OAB): The brain’s inhibition fails, causing sudden, strong urges to urinate.
- Urinary retention: Signals to contract the bladder are weak, so the organ fills beyond capacity.
- Stress incontinence: Loss of pelvic floor control when coughing or moving.
- Mixed dysfunction: A combination of urgency and retention, which is the most confusing for patients.
These patterns often appear within the first 48 hours after surgery but can emerge weeks later as swelling resolves or medications wear off.
Red Flags: When to Call a Doctor Immediately
- Inability to pass any urine for more than six hours.
- Severe lower‑abdominal pain that feels like a full bladder.
- Fever, chills, or foul‑smelling urine-signs of a urinary tract infection (UTI) that can quickly complicate brain recovery.
- Sudden, continuous leakage that interferes with wound dressings or catheter sites.
Each of these symptoms signals a possible blockage, infection, or worsening neuro‑control that needs prompt assessment.
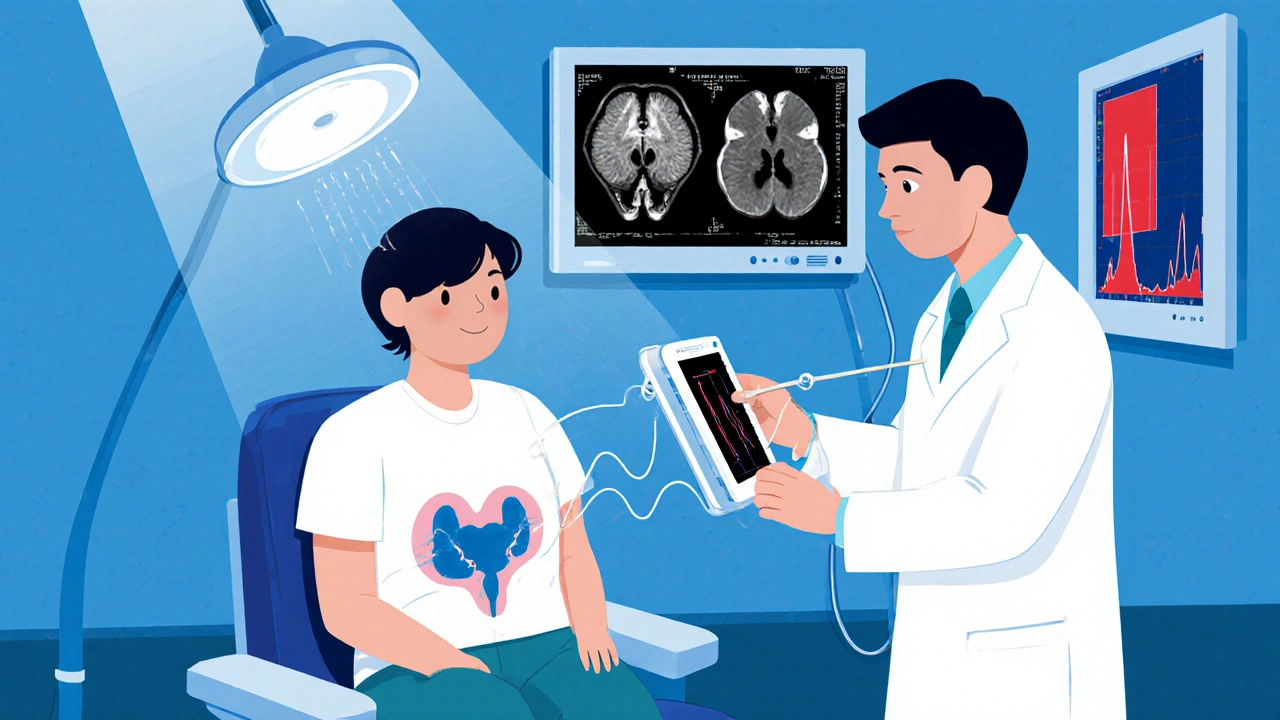
Diagnostic Steps: From Simple Checks to High‑Tech Tests
Doctors start with the basics, then move to specialized studies if the problem persists.
| Step | What It Looks Like | Why It Matters |
|---|---|---|
| Urinalysis | Dip‑stick test for blood, glucose, leukocytes | Rules out infection or metabolic causes |
| Post‑void residual (PVR) scan | Ultrasound measurement after voiding | Quantifies retention - >150 mL is concerning |
| Urodynamic testing | Urodynamic testing | Measures bladder pressure, flow rates, and sphincter activity to pinpoint neurogenic patterns |
| Neuro‑imaging | CT or MRI of the brain | Identifies lesions like subdural hematoma that can compress the micturition centers |
Management Options: What Works and When
Treatment is a mix of short‑term relief and long‑term rehabilitation.
- Intermittent catheterization: A clean technique performed every 4-6 hours to prevent bladder over‑distension. It’s the gold standard for acute retention.
- Anticholinergic medication: Drugs like oxybutynin relax the bladder muscle, reducing urgency. They’re most effective when OAB dominates the picture.
- Bladder training: A structured schedule-trying to void every 2-3 hours-re‑educates the brain‑spinal circuit. Works best after the acute phase.
- Pelvic floor physical therapy: Targeted exercises strengthen the sphincter and improve sensation, especially useful for stress incontinence.
- Neuromodulation: Electrical stimulation of sacral nerves (SNS) can reset faulty pathways when meds fail.
Choosing the right approach depends on the dominant symptom, the patient’s overall health, and the presence of comorbidities like Parkinson’s disease or spinal injuries.
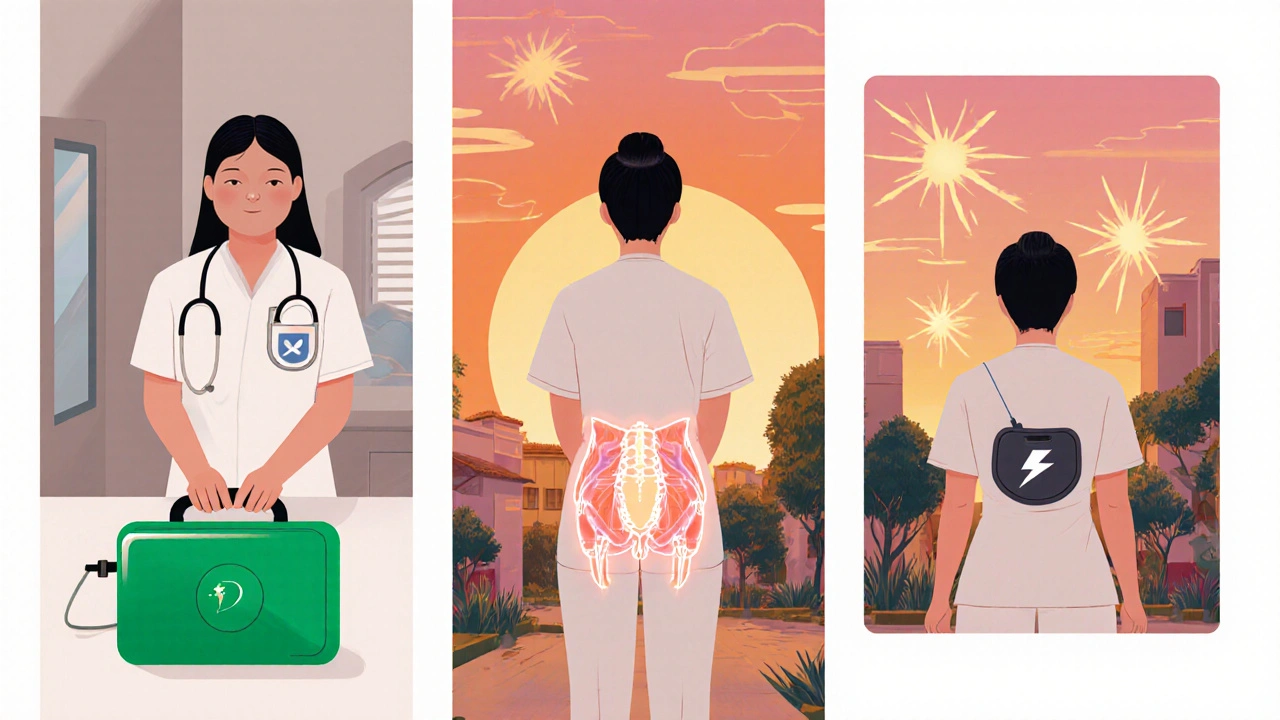
Prevention and Post‑Operative Care Tips
Even before surgery, a few steps can reduce the likelihood of severe urinary fallout.
- Discuss bladder‑control history with the neurosurgeon-prior UTIs, prostate issues, or known neurogenic problems matter.
- Ask the anesthesiology team about minimizing anticholinergic drugs that may mask early signs.
- Arrange for bedside bladder scans within 24 hours after the operation.
- Keep a fluid‑intake log; too much caffeine or alcohol can aggravate OAB.
- Start gentle pelvic floor exercises as soon as the surgeon clears you-often the day after surgery.
Early vigilance turns a potentially permanent problem into a manageable, short‑term inconvenience.
Quick Checklist for Patients and Caregivers
- Monitor urine frequency and volume every shift.
- Record any leakage, urgency, or inability to void.
- Report pain or a full‑bladder feeling immediately.
- Ensure a clean intermittent catheter kit is on hand if prescribed.
- Schedule a follow‑up urodynamic study before discharge if symptoms persist.
Keeping this list visible on the bedside table helps everyone stay on the same page.
Bottom Line
Urinary problems after head surgery or trauma aren’t just an annoyance; they’re a window into the nervous system’s health. Spotting the signs early, running the right tests, and applying targeted therapies can prevent long‑term bladder dysfunction and speed overall recovery. If you or a loved one has just undergone a craniotomy or suffered a severe head hit, treat any change in bathroom habits with the same seriousness you’d give a fever or wound infection.
Why do headaches sometimes cause more bathroom trips?
Head injuries can irritate the pontine micturition center, which increases urgency signals. The brain may mistake pressure changes as a need to void, leading to frequent trips.
Is it safe to use over‑the‑counter bladder pills after brain surgery?
Most OTC anticholinergics can interact with anesthesia or other post‑op meds. Always get a physician’s approval before adding any bladder‑control drug.
How long does intermittent catheterization usually last?
For acute retention, it’s typically 1‑2 weeks until the bladder regains normal sensation. Some patients need it longer if nerve recovery is slow.
Can pelvic floor exercises help if I have a subdural hematoma?
Yes-once the neurosurgeon clears you for movement, gentle Kegel‑type contractions strengthen the sphincter and can reduce stress incontinence, even with a subdural bleed.
What’s the difference between a UTI and neurogenic bladder symptoms?
A UTI usually brings fever, burning on urination, and cloudy urine. Neurogenic bladder causes urgency, retention, or leakage without infection signs. A urine test separates the two.

14 Comments
If you ignore bladder issues after a craniotomy you're basically signing up for lifelong trouble.
The neurogenic bladder phenomenon is a classic example of how central and peripheral pathways intertwine. When the pontine micturition center gets disrupted, you see a cascade of urgency, retention, and sometimes incontinence. Early urodynamic profiling can delineate detrusor overactivity from underactivity, guiding whether anticholinergics or intermittent catheterization are indicated. Integrating pelvic‑floor physiotherapy early on also helps re‑establish sphincter coordination, especially in mixed dysfunction cases.
Wake up, people! The pharma industry doesn’t want you to know that most of these bladder meds are just placebos draped in conspiracy. They profit from keeping you dependent while ignoring the real brain‑spinal cord damage that’s been hidden from the public.
I hear your frustration, Theo, but the reality is that most post‑operative urinary issues stem from predictable neuro‑physiology, not shadowy cabals. Addressing them with evidence‑based protocols-like scheduled bladder scans and timely catheter removal-offers the safest path to recovery.
It is incumbent upon clinicians to perform a thorough post‑operative urinalysis and post‑void residual measurement before deeming any urinary dysfunction as purely neurogenic. This systematic approach mitigates the risk of overlooking a treatable infection.
Team, remember that consistent bladder training can rewire those neural circuits faster than you think. Set a timer, stick to a schedule, and watch the urgency waves subside. You’ve got the power to take control of your recovery.
The author overlooks the socioeconomic dimension: patients without access to clean intermittent catheter kits are at higher risk for iatrogenic complications. Moreover, the recommendation to start pelvic floor exercises "as soon as cleared" fails to consider resource‑limited settings where physiotherapy is scarce.
Indeed, equitable access to bladder management tools is essential. Hospitals should proactively provide disposable catheter kits and ensure that bedside ultrasound devices are available for all postoperative patients, irrespective of insurance status. 😊
Oh sure, because the government totally cares about your bladder after a head injury. They’ll probably just replace your catheters with Wi‑Fi enabled drones, right? 🙄
Yep, totally trust the system. 😂
Let’s collab on a shared checklist template that we can all upload to the ward board. Having a unified visual cue will reduce missed urine outputs and streamline communication between nurses and physicians.
From a cultural standpoint, many patients view urinary incontinence as a taboo, which can delay reporting. By normalizing the conversation and embedding education into discharge planning, we empower patients to seek help without shame.
Wow, another “expert” telling us to do bladder scans. Because we totally have a spare ultrasonographer on every floor, right?
Listen up, folks! The reality of post‑cranial trauma urinary dysfunction is far more intricate than any checklist can capture. First, you must recognize that the pontine micturition center does not operate in isolation; it is a hub within a distributed network that includes the periaqueductal gray, the insular cortex, and even limbic structures that modulate emotional responses to bladder filling. When any node in this circuitry is compromised-whether by edema, hemorrhage, or surgical manipulation-the downstream effect is a loss of synchrony between detrusor contraction and sphincter relaxation. This desynchrony manifests clinically as either detrusor overactivity, producing urgency and frequency, or detrusor underactivity, leading to retention and overflow incontinence. It is therefore imperative to perform a comprehensive urodynamic study within the first week post‑injury to map the pressure‑flow relationships and identify the precise phenotype. Second, the management algorithm should not be a one‑size‑fits‑all; anticholinergic agents like oxybutynin are contraindicated in patients with concomitant cognitive impairment because they exacerbate delirium, whereas beta‑3 agonists may provide a safer profile. Third, intermittent catheterization, while gold‑standard for acute retention, must be paired with meticulous aseptic technique and scheduled catheter changes to prevent catheter‑associated urinary tract infections, which can further impair neuro‑recovery. Fourth, the role of sacral neuromodulation-though still emerging-offers a promising avenue for patients with refractory neurogenic bladder, but it requires multidisciplinary coordination between neurosurgeons, urologists, and rehabilitation specialists. Fifth, psychosocial support is non‑negotiable: patients often experience profound embarrassment and isolation, which can delay reporting of symptoms and hinder adherence to therapy. Integrating a mental‑health professional into the care team ensures that these concerns are addressed promptly. Finally, education of caregivers cannot be overstated; they should be trained to recognize red‑flag signs such as a suprapubic fullness, new‑onset fever, or sudden increase in leakage, and to act without hesitation. By embracing this comprehensive, nuanced approach-grounded in neuroanatomy, evidence‑based pharmacology, and compassionate care-we can transform a potentially debilitating sequela into a manageable, reversible condition.
Write a comment