Stress & Bloating Tracker
Click on any trigger below to see its potential impact on your gut:
Mindfulness Meditation
10-20 minutes dailyLowers cortisol and improves vagal tone
Deep Breathing
5-10 minutes per sessionActivates parasympathetic system, speeds transit
Your Personalized Insight
Select a stress trigger and adjust the bloating level to see personalized insights.
Key Takeaways
- Stress can cause or worsen abdominal distension through hormonal and neural pathways.
- The gut‑brain axis is the main highway linking emotional stress to digestive symptoms.
- Simple lifestyle tweaks-mindfulness, breath work, diet tweaks-can dramatically cut bloating.
- Identifying personal stress triggers helps you choose the right management tools.
- Consistent practice of at least two stress‑reduction techniques yields noticeable relief within weeks.
What Is Abdominal Distension?
People often call it “bloating,” but medically abdominal distension refers to a visible or measurable increase in stomach size caused by excess gas, fluid, or slowed motility. It can feel tight, uncomfortable, and may be accompanied by pain, belching, or changes in bowel habits.
Typical causes include overeating, high‑FODMAP foods, constipation, and certain medications. However, a less obvious driver is psychological stress, which can kick‑start a cascade of gut reactions even when you haven’t eaten anything unusual.
How Stress Triggers Bloating
When you encounter a stressor-tight deadline, argument, or even chronic anxiety-your brain activates the sympathetic nervous system. This “fight‑or‑flight” response releases hormones like adrenaline and cortisol that alter gut function.
Key effects include:
- Reduced blood flow to the intestines, slowing digestion.
- Increased intestinal permeability, allowing gas‑producing bacteria to thrive.
- Heightened sensitivity of the enteric nervous system, making you feel bloated even with small gas volumes.
These changes often linger after the stressful moment ends, creating a feedback loop where the gut feels perpetually “on edge.”
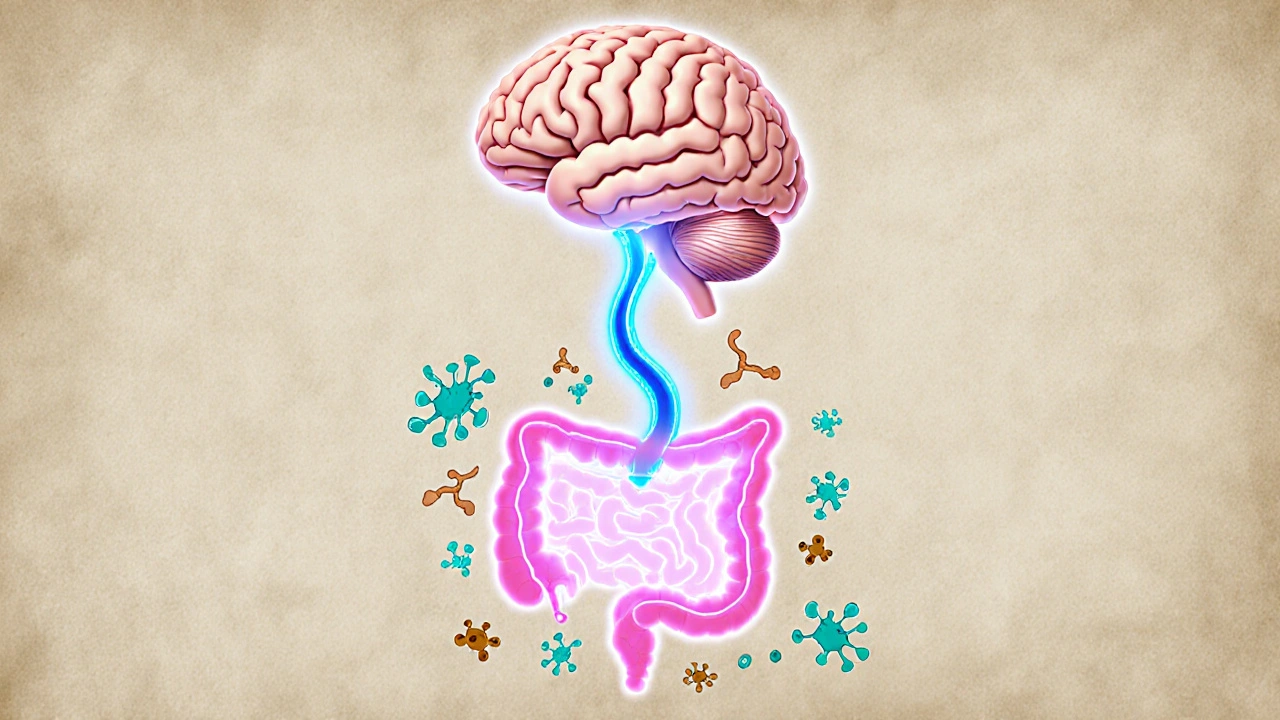
The Gut‑Brain Axis: Your Body’s Two‑Way Street
The gut‑brain axis is a bi‑directional communication network linking the central nervous system and the enteric nervous system. It uses neural pathways (vagus nerve), hormones, and immune signals.
When stress spikes, it sends signals down the vagus nerve, prompting the gut to slow motility and hold onto gas. At the same time, gut microbes release metabolites that can influence mood, completing a loop that keeps both brain and belly on high alert.
Hormonal Pathways: Cortisol and Its Effects
Cortisol is the primary stress hormone. Short‑term spikes help you cope, but chronic elevation disrupts the gut in several ways:
- It increases the production of gastric acid, leading to irritation and gas.
- It alters the composition of the microbiome, favoring gas‑producing strains like Clostridium spp.
- It slows colonic transit, giving microbes more time to ferment undigested carbohydrates.
Measuring cortisol via a simple saliva test can confirm whether stress is a hidden driver of your bloating.
Common Conditions Linked to Stress‑Induced Distension
Several digestive disorders worsen under stress:
- Irritable Bowel Syndrome (IBS): 60‑70% of IBS patients report symptom flare‑ups during stressful periods.
- Functional dyspeasia: stress amplifies stomach pain and fullness.
- Small‑intestinal bacterial overgrowth (SIBO): stress‑related motility slowdown creates a breeding ground for bacteria.
- Acid reflux: higher cortisol levels can relax the lower esophageal sphincter, leading to belching and bloating.
Practical Ways to Manage Stress and Reduce Bloating
Below is a quick‑reference table of evidence‑based stress‑reduction tools that also show measurable benefits for gut comfort.
| Technique | Typical Session Length | Primary Gut Benefit |
|---|---|---|
| Mindfulness meditation | 10‑20minutes daily | Lowers cortisol, improves vagal tone |
| Diaphragmatic breathing | 5‑10minutes per session | Activates parasympathetic system, speeds transit |
| Gentle yoga (e.g., Hatha) | 30minutes, 3‑4times/week | Reduces abdominal muscle tension, balances microbiome |
| Progressive muscle relaxation | 15minutes before bedtime | Decreases anxiety‑driven gut hypersensitivity |
| Regular aerobic walk | 20‑30minutes, most days | Boosts overall GI motility, cuts inflammatory markers |
Pick two techniques that fit your schedule and try them consistently for at least two weeks. Many users notice a 15‑30% reduction in bloating severity within that timeframe.
Diet Tweaks That Complement Stress Management
While stress reduction is the cornerstone, small dietary adjustments amplify results:
- Limit high‑FODMAP foods (e.g., onions, garlic, beans) on especially stressful days.
- Include Probiotics with strains like Lactobacillus plantarum, shown to lower stress‑related gas production.
- Stay hydrated-water helps move waste and dilute gastric acid.
- Eat slowly, chewing each bite 20‑30 times to activate digestive enzymes before the gut is stressed.
Creating a Personal Action Plan
Follow this three‑step framework to turn knowledge into relief:
- Identify Triggers: Keep a one‑week journal noting stress events, meals, and bloating intensity on a scale of 1‑10.
- Pick Tools: Choose two stress‑reduction techniques from the table and a probiotic supplement that suits your regimen.
- Measure Progress: Re‑evaluate your bloating score after two weeks. Adjust session length or add another technique if improvement stalls.
Consistency beats intensity. Even five minutes of breath work each morning can shift the hormonal balance enough to ease gas buildup.
When to Seek Professional Help
If bloating persists despite lifestyle changes, consider these next steps:
- Visit a gastroenterologist for tests like a hydrogen breath test (checks SIBO) or a stool analysis (microbiome profile).
- Talk to a mental‑health professional about chronic anxiety; cognitive‑behavioral therapy (CBT) has a 40‑60% success rate in reducing stress‑related GI symptoms.
- Review any medication list; some drugs (e.g., opioids, anticholinergics) can impair gut motility.
Frequently Asked Questions
Can occasional stress really cause noticeable bloating?
Yes. Even brief spikes in cortisol can slow intestinal transit for a few hours, leading to gas accumulation. Most people feel the effect within 30‑60 minutes after a stressful event.
How does mindfulness specifically help the gut?
Mindfulness lowers sympathetic activation, allowing the vagus nerve to restore its calming influence on digestion. Studies show a 20% drop in self‑reported bloating after an eight‑week mindfulness program.
Are probiotics effective for stress‑related abdominal distension?
Certain strains, especially Lactobacillus plantarum and Bifidobacterium infantis, have been shown to reduce cortisol levels and gas production. A daily dose of 10‑20billion CFU for four weeks often yields improvement.
Should I avoid coffee if I’m stressed and bloated?
Caffeine can increase acid secretion and trigger the stress response, worsening bloating for some people. If you notice a pattern, try swapping with decaf or herbal tea for two weeks and track the difference.
How long does it take to see results from stress‑reduction practices?
Most individuals report noticeable relief after 7‑14 days of consistent practice. Full adaptation-where the gut no longer overreacts-can take 4‑6 weeks.


17 Comments
Keeping it easy, stress can make your belly feel weird but a short walk helps.
Ah, the delightful dance of cortisol and gas bubbles, a masterpiece of modern misery that turns your gut into a carnival of chaos.
When work deadlines loom, your sympathetic nervous system fires up like a reckless fireworks display, slamming the brakes on gastric motility while simultaneously inflating the intestinal balloons with trapped air.
Family arguments are the perfect culinary sabotage, weaving emotional knots that tighten the sphincters and trap every piece of indigestion in a vicious vortex.
Financial worries, those relentless whispering gremlins, hijack your hypothalamic‑pituitary‑adrenal axis, dumping a flood of stress hormones that love nothing more than to ferment carbs into snarling bloating.
Health concerns, especially those chronic conditions, act like a silent puppeteer, pulling strings that make the vagus nerve twitch in protest, slowing transit and inviting unnecessary fermentation.
All of this creates a perfect storm where the gut’s microbiome becomes a hostile battlefield, with bad bacteria thriving on the excess sugars and stress‑induced mucus.
The colon, once a tranquil river, now resembles a clogged sewer, and each passage is accompanied by a symphony of gurgles that echo your inner turmoil.
But fear not, for the body is a resilient wonder; mindfulness meditation can gently coax the cortisol levels down, allowing the gut to breathe again.
Deep breathing, a simple yet profound tool, reactivates the parasympathetic system, coaxing the intestinal muscles to contract in a coordinated ballet.
Probiotics, especially multi‑strain formulations, can repopulate the gut with beneficial microbes that outcompete the gas‑producing villains.
Regular light exercise, such as a 20‑minute brisk walk, serves as a mechanical agitator, nudging the trapped air and waste through the intestines.
Hydration, often overlooked, acts as a lubricant, ensuring that the digestive tract remains slick and efficient.
Dietary adjustments, like reducing fermentable oligosaccharides, can deprive the gas‑producing bacteria of their favorite feast.
Sleep, the unsung hero, restores the hormonal balance, giving the gut a chance to reset its rhythm.
Ultimately, the interplay between mind and gut is a two‑way street; nurturing one side inevitably benefits the other, turning that uncomfortable distension into a manageable footnote.
I’ve felt the pressure of a deadline creep into my stomach, making it feel like a balloon about to pop.
From a philosophical angle, stress is a perturbation to the body’s equilibrium, and the gut is a sensitive barometer of that disturbance.
So you’re telling me a coffee-fueled email marathon can literally puff you up like a hamster in a wheel? Brilliant.
Actually, incorporating a daily probiotic regimen alongside mindfulness can significantly reduce cortisol‑induced bloating; many patients report noticeable improvement within two weeks.
Honestly, if you’re not tracking every single bite and stress trigger, you’re just playing Russian roulette with your gut – and that’s drama at its finest.
Let’s take a collaborative approach: start a daily journal noting stress sources, meal composition, and bowel movements; over time, patterns emerge, and you can fine‑tune interventions like timed breathing exercises or low‑FODMAP meals to target the most disruptive factors.
Great point! Journaling is a low‑cost, high‑yield strategy; just remember to log the exact timing of stress events and the subsequent bloating intensity – the data will speak for itself!!
👍 Remember to use consistent units (e.g., severity 1‑10) and avoid ambiguous terms; this keeps your dataset clean for any future statistical analysis. 😊
From an inclusive health education perspective, it’s essential to acknowledge that socioeconomic stressors can exacerbate gastrointestinal symptoms, and providing accessible resources like free community workshops on stress reduction can empower individuals to take proactive steps toward gut health.
Sure, but don’t you think the whole “stress‑bloating” narrative is just a distraction from the real agenda: big pharma pushing unnecessary supplements onto unsuspecting consumers?
While it’s easy to default to conspiratorial thinking, the evidence base for probiotic efficacy in stress‑related bloating is actually robust, with multiple randomized controlled trials demonstrating measurable reductions in abdominal girth and subjective discomfort.
One must consider the moral implications of ignoring gut‑brain axis research; if we dismiss scientifically‑backed interventions, we’re effectively endangering public health under the guise of personal responsibility.
Absolutely, taking a balanced view and encouraging evidence‑based practices can help people feel both empowered and safe.
In many cultures, mindfulness and breath work have been integral to digestive wellness for centuries, and integrating these practices with modern medical guidance creates a holistic framework that respects both tradition and science.
Honestly, if you’re not skeptical about every health claim, you’re just another pawn in the wellness industry’s game – but hey, maybe a little drama adds spice to the bland routine of self‑care.
Write a comment