PPI and Antifungal Interaction Checker
Select a PPI and antifungal to check their interaction.
When you take a proton pump inhibitor (PPI) for heartburn and an antifungal for a stubborn yeast infection at the same time, you might think you’re doing everything right. But what if those two pills are secretly working against each other? It’s not just a theory-it’s a well-documented problem that affects real patients every day. The interaction between PPIs and certain antifungals can drop drug levels so low that treatment fails, leading to longer infections, hospital stays, and higher costs. And here’s the twist: some newer research suggests PPIs might actually help antifungals work better in other ways. This isn’t just about avoiding bad combos-it’s about understanding a complex, two-sided relationship that’s changing how doctors prescribe.
Why PPIs Mess With Antifungal Absorption
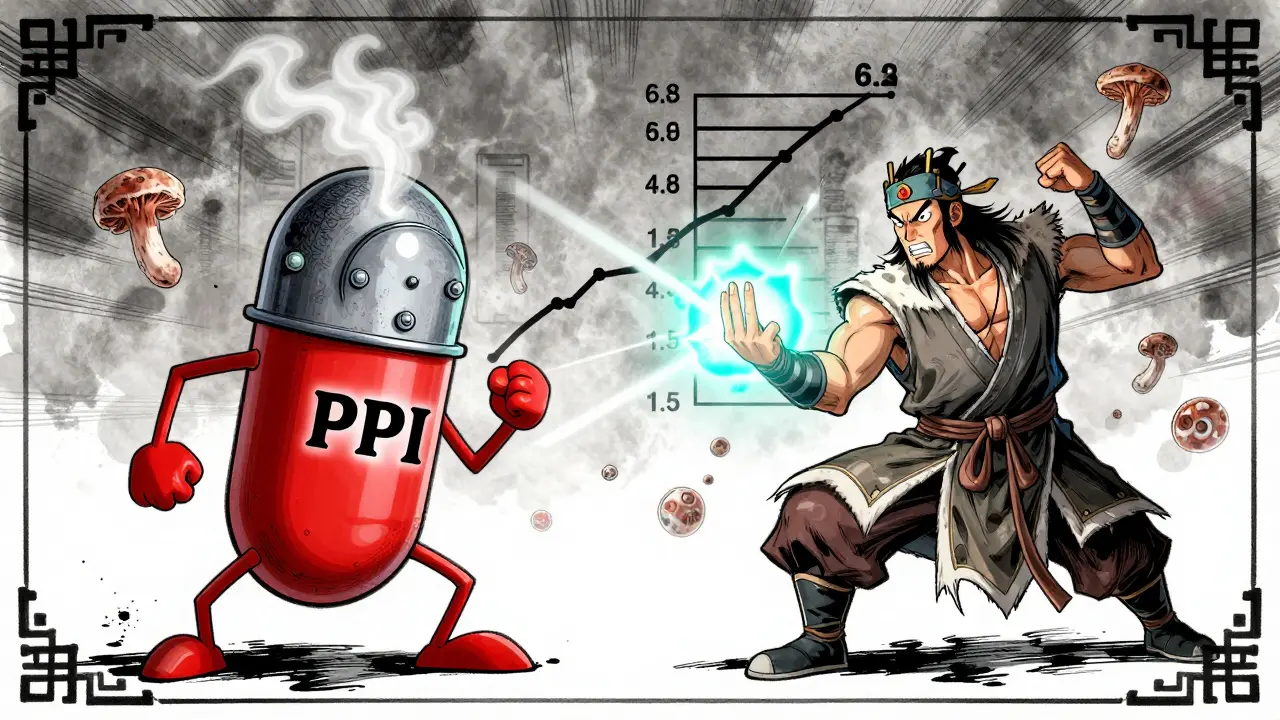
Proton pump inhibitors like omeprazole, pantoprazole, and esomeprazole work by shutting down the stomach’s acid production. That’s great for reducing heartburn, but it creates a problem for drugs that need acid to dissolve. Two major antifungals-itraconazole and ketoconazole-rely on a low-pH environment to be absorbed properly. When you take a PPI, your stomach pH rises from around 1.5 to 4 or even 6. That small change makes a huge difference.At pH 1.2, ketoconazole dissolves at 22 mg/mL. At pH 6.8, that drops to just 0.02 mg/mL. Itraconazole isn’t much better. A 2023 study in JAMA Network Open tracking over 1,200 patients found that when PPIs were taken with itraconazole, the amount of drug absorbed dropped by 60%. That’s not a minor dip-it’s enough to push blood levels below the minimum needed to kill fungi. The FDA added a black box warning to itraconazole in 2023, clearly stating: concomitant use with PPIs is contraindicated.
Fluconazole, on the other hand, doesn’t care. It’s highly water-soluble and absorbs just fine whether your stomach is acidic or not. Its bioavailability stays around 90% regardless of pH. That’s why fluconazole is often the go-to antifungal when PPIs are needed. But even that’s not the whole story.
The Hidden Metabolic Battle
It’s not just about stomach acid. Both PPIs and antifungals are processed by the same liver enzymes-cytochrome P450. That’s where things get messy. Ketoconazole and itraconazole are almost entirely broken down by CYP3A4. But so is lansoprazole and omeprazole. When they’re taken together, they compete. The result? Either the antifungal doesn’t get broken down fast enough, or the PPI doesn’t activate properly.Voriconazole adds another layer. It’s metabolized by CYP2C19 and CYP3A4. PPIs like pantoprazole and omeprazole block CYP2C19. That means voriconazole sticks around longer than it should. A 2015 study showed PPIs reduce voriconazole clearance by 25-35%. That might sound good-until you realize it raises the risk of toxicity. Side effects like vision changes, liver damage, and skin rashes become more likely.
Fluconazole doesn’t rely on CYP3A4, but it’s a strong inhibitor of CYP2C9. That’s the enzyme that breaks down warfarin, some diabetes drugs, and NSAIDs. So even if fluconazole plays nice with PPIs on the absorption front, it can still cause dangerous interactions with other medications you’re taking.

The Paradox: PPIs Might Help Antifungals Work Better
Here’s where it gets surprising. A 2024 study published in PMC10831725 found something unexpected: omeprazole and other PPIs can directly interfere with a fungal protein called Pam1p-a plasma membrane ATPase that Candida uses to pump out antifungal drugs. When that pump is blocked, the fungus can’t get rid of fluconazole as easily. In lab tests, adding omeprazole to fluconazole reduced the minimum dose needed to kill resistant Candida glabrata by 4 to 8 times.This isn’t just a lab curiosity. Researchers at Johns Hopkins are now running a Phase II trial (NCT05876543) testing whether low-dose omeprazole can boost fluconazole’s power in patients with stubborn fungal infections. If it works, we could be looking at a new way to treat drug-resistant candidiasis without needing stronger, more toxic drugs.
But here’s the catch: this effect hasn’t been proven in people yet. The absorption problem is real and immediate. The synergy effect is promising but still experimental. So right now, you can’t rely on PPIs to help your antifungal work better-you have to assume they’ll hurt it.
What Doctors Do When Both Drugs Are Needed
If you’re on a PPI and need an antifungal, your doctor won’t just pick one at random. They’ll look at your situation and choose the safest path.For itraconazole and ketoconazole? Avoid them completely if you’re on a PPI. Most hospitals and clinics now use echinocandins like caspofungin as the go-to alternative for serious fungal infections in patients taking acid reducers. They’re given intravenously, so stomach pH doesn’t matter.
If you absolutely must use itraconazole, timing matters. UCSF’s protocol says to take it at least two hours before the PPI. Mayo Clinic recommends a 4-6 hour gap. But even then, absorption still drops by 45%. That’s why therapeutic drug monitoring is critical-blood tests to check if drug levels are in the safe, effective range (0.5-1.0 μg/mL for itraconazole).
For voriconazole, it’s about monitoring. If you start a PPI while on voriconazole, your levels will rise. Your pharmacist or doctor will check your blood levels within 72 hours and adjust your dose by 25-50% to avoid toxicity.
And fluconazole? It’s usually fine. But if you’re also on warfarin, your INR needs closer watching. Fluconazole can make warfarin stronger, raising your risk of bleeding. A 20-30% reduction in warfarin dose is often needed.

Why This Matters More Than You Think
These aren’t rare edge cases. In 2023, over 18.7% of hospitalized patients got both a PPI and a systemic antifungal. That’s nearly 1 in 5. A 2024 study in JAMA Internal Medicine found that improper combinations like this cost the U.S. healthcare system $327 million a year-mostly from longer hospital stays, repeat treatments, and complications from treatment failure.And despite warnings, a 2024 audit found that over 22% of itraconazole prescriptions in community pharmacies were still being written with PPIs. That’s not just a mistake-it’s a systemic gap in education. Many prescribers still don’t realize how severe this interaction is.
What’s Coming Next
The future is moving toward solutions that bypass the problem entirely. The FDA is funding research into new formulations of itraconazole that don’t need stomach acid to work. One submicron version, SUBA-itraconazole, showed 92% bioavailability even with a PPI in a 2023 trial. That’s a game-changer.Meanwhile, scientists are exploring whether we can repurpose PPIs as antifungal boosters. If the ongoing Johns Hopkins trial succeeds, we might soon have a new treatment strategy: low-dose omeprazole + fluconazole for resistant fungal infections.
But until those options are widely available, the rule is simple: don’t mix itraconazole or ketoconazole with PPIs. Use fluconazole if possible. Monitor voriconazole levels closely. And always tell your doctor and pharmacist exactly what you’re taking.
Can I take fluconazole with a proton pump inhibitor?
Yes, fluconazole can be safely taken with proton pump inhibitors. Unlike itraconazole or ketoconazole, fluconazole doesn’t rely on stomach acid for absorption-it’s highly water-soluble and absorbs well at any pH. Its bioavailability stays around 90% regardless of whether you’re on omeprazole, pantoprazole, or another PPI. The main concern with fluconazole isn’t the PPI-it’s that fluconazole can interfere with other medications like warfarin, so your doctor may need to adjust those doses.
Why is itraconazole contraindicated with PPIs?
Itraconazole needs an acidic environment in the stomach to dissolve and be absorbed. Proton pump inhibitors raise stomach pH, which reduces itraconazole absorption by up to 60%. This can drop blood levels below the minimum needed to fight fungal infections, leading to treatment failure. Because of this, the FDA added a black box warning in 2023, making it clear that combining itraconazole with PPIs is contraindicated.
What antifungal can I use instead of itraconazole if I’m on a PPI?
Echinocandins like caspofungin, micafungin, or anidulafungin are the preferred alternatives. They’re given intravenously, so stomach pH doesn’t affect them. For oral treatment, fluconazole is often used if the infection is susceptible. Voriconazole can be used too, but only with careful blood level monitoring, since PPIs can increase its concentration and raise the risk of side effects.
Do PPIs affect all antifungals the same way?
No. Only pH-dependent antifungals like itraconazole and ketoconazole are affected by PPIs in terms of absorption. Fluconazole is unaffected. Voriconazole isn’t impacted in absorption but its metabolism is slowed by PPIs, leading to higher blood levels. The effect varies by drug, so it’s not a one-size-fits-all interaction.
Is there any benefit to taking PPIs with antifungals?
Emerging research suggests PPIs like omeprazole may help antifungals like fluconazole work better against resistant Candida by blocking a fungal pump that ejects the drug. This has been shown in lab studies and is now being tested in clinical trials. But this effect hasn’t been proven in patients yet. Until then, the risk of reduced absorption outweighs any potential benefit, so combining them isn’t recommended outside of controlled studies.

15 Comments
This is why people die from simple infections. You think you're just popping a pill for heartburn, but you're basically handing your immune system a suicide note. PPIs are overprescribed like candy, and doctors act like they're harmless. I've seen patients get sepsis because some lazy GP threw them on omeprazole and then prescribed itraconazole without checking interactions. It's not just ignorance-it's negligence. The FDA warning is there for a reason, and yet pharmacies still fill these combos like it's normal. Someone needs to sue the pharmaceutical industry into oblivion.
Of course the government wants you to think this is a 'drug interaction.' What they're not telling you is that PPIs are a Trojan horse for Big Pharma's real agenda: keeping you dependent on expensive antifungals. If your stomach acid was allowed to do its job, you wouldn't need drugs at all. Natural remedies work. Garlic. Coconut oil. Apple cider vinegar. But why would the FDA endorse that? It doesn't make money. This whole thing is a scam to sell you more pills. And now they want to use PPIs to boost antifungals? That's just a new way to lock you into the system. Wake up, sheeple.
okay but like… what if i just stop taking the ppi? i’ve had acid reflux since college and i’ve been on pantoprazole for 8 years. i tried quitting once and felt like my esophagus was on fire for a week. also my mom had a fungal infection and they gave her fluconazole and it worked fine. so… is this just a problem for rich people who take fancy drugs? 🤔
Thank you for writing this. I’ve been a nurse for 15 years and I’ve seen too many patients get worse because of these interactions. I always double-check med lists, but not every provider does. Fluconazole is usually the safe bet, but even then-watch for warfarin. I’ve had patients bleed out because no one connected the dots. Please, if you’re on any of these meds, talk to your pharmacist. They’re the unsung heroes here. And if your doctor dismisses you? Get a second opinion. Your life matters more than a quick fix for heartburn.
The real tragedy isn’t the drug interaction-it’s the reductionist thinking that got us here. We treat biology like a vending machine: insert pill, get relief. But the body is a symphony, not a switchboard. PPIs suppress acid, but acid isn’t just for digestion-it’s a gatekeeper. When you silence it, you don’t just disrupt absorption-you disrupt microbial balance, immune signaling, nutrient cycling. And now we’re trying to weaponize the very thing we suppressed to fix the damage? That’s not medicine. That’s alchemy with a DEA license.
so like… if i take my ppi at night and my itraconazole in the morning… is that cool? 🤷♂️ i did it for 3 weeks and my yeast didn’t get worse but my stomach still burns. also why does everyone say ‘PPI’ like it’s a bad word? i’m not a villain, i just have acid reflux. 😭
Clear, evidence-based, and clinically essential. The data on absorption and metabolism is unambiguous. Fluconazole remains the preferred oral agent in patients on PPIs. For itraconazole, therapeutic drug monitoring is non-negotiable. Echinocandins are appropriate for severe infections. The emerging synergy with omeprazole is promising but requires validation. Until then, adherence to established guidelines prevents harm.
Let’s be brutally honest: this isn’t about pharmacokinetics. It’s about power. The medical-industrial complex doesn’t want you to know that a $0.10 generic PPI might one day be repurposed to reverse antifungal resistance. They profit from expensive IV antifungals, from repeated hospitalizations, from lifelong prescriptions. The ‘contraindication’ is a legal shield, not a scientific truth. The real enemy isn’t the drug interaction-it’s the system that profits from your ignorance. And now they’re testing a combo that could break their business model? Of course it’s in Phase II. It’s not about healing. It’s about control.
Everything is connected. Stomach acid isn’t waste-it’s a signal. Suppressing it changes the microbiome, alters immune response, affects nutrient uptake. The antifungal interaction is just one symptom. The real question: why are we suppressing acid at all? Is heartburn a disease… or a warning?
i live in a country where fluconazole is sold over the counter and ppi's are basically bottled water... so i just took them together for months and nothing happened? 🤷♀️ maybe it's different for people who are sick or old? i just feel bad for those who are scared to take meds because of all this. can someone explain what the actual risk is for a healthy 30 year old? 🙏
This is such an important topic-and you’ve explained it with such clarity. I’ve had patients panic because they were told they couldn’t take their heartburn medication while on antifungals. It’s reassuring to know fluconazole is safe. Thank you for including practical guidance and alternatives. Healthcare should be this clear. Please keep writing. This kind of information saves lives.
It’s a classic case of pharmaceutical reductionism. You isolate a single variable-gastric pH-and assume causality, ignoring the emergent properties of systemic homeostasis. The CYP450 interplay is not merely competitive inhibition; it’s a dynamic equilibrium shaped by epigenetic modulation, gut-liver axis signaling, and microbial metabolite flux. The clinical guidelines are outdated because they’re rooted in pharmacodynamic silos, not systems biology. Until we model the organism as a whole, we’re just rearranging deck chairs on the Titanic.
Everyone is making this too complicated. I took ketoconazole and omeprazole together when I was in India and nothing happened. My fungus went away. My stomach was fine. The problem is not the drugs. The problem is doctors in America overthinking everything. They want to make money from blood tests and IV drugs. In my country, we just use what works. If you are not sick, you don’t need all this monitoring. Just take the pills and stop worrying. Science is not a religion. If it worked for me, it can work for you.
They’re trying to scare you with ‘black box warnings’ so you’ll pay for expensive IV drugs instead of cheap pills. This is all a scam. PPIs are safe. Fluconazole is safe. The real enemy is the medical elite who want to control your health. If you’re not in a hospital, you don’t need a blood test. Take your meds, trust your body, and stop listening to fear-mongering blogs. America is turning healthy people into patients. Don’t fall for it.
What if the PPI-antifungal interaction isn’t a mistake… but a feature? What if the system is designed to create chronic fungal overgrowth so we keep buying drugs? Think about it-PPIs are prescribed for GERD, but GERD is often caused by low stomach acid, not high. The whole diagnostic model is inverted. The fungi thrive because the environment is altered. The drugs are made to treat the symptoms of the drugs. It’s a closed loop. They don’t want to fix the root cause-they want to monetize the cascade. The Johns Hopkins trial? It’s not about healing. It’s about patenting a new combo before the old one becomes obsolete. Welcome to pharmacological dystopia.
Write a comment