Medication Error vs. Side Effect Quiz
Test Your Knowledge
You were prescribed 10 mg of medication, but you received 20 mg.
You took your antihistamine for allergies and felt drowsy.
You were told to take your blood pressure medication with food, but you took it on an empty stomach and felt dizzy.
You're taking an antibiotic and developed nausea.
You were given a medication that had expired last month.
You're taking a statin for cholesterol and experienced muscle pain.
Every year, over 1.3 million people in the U.S. are injured because of problems with their medications. Some of these are mistakes. Others are side effects. And too often, people - even doctors and nurses - mix them up. That’s dangerous. If you think a reaction is just a side effect when it’s actually a medication error, you’re not fixing the real problem. And if you blame the drug when it was a human or system error, you’re missing a chance to prevent the next one.
What’s the difference between a medication error and a side effect?
A medication error is something that went wrong in the process of giving you the drug. It’s preventable. It could be the wrong dose, the wrong pill, the wrong time, or even the wrong patient. Think of it like ordering a coffee and getting tea instead. The tea isn’t bad - you just didn’t get what you asked for.
A side effect is something that happens because of the drug, even when everything is done right. It’s not a mistake. It’s a known, expected reaction that wasn’t the goal. For example, if you take an antihistamine for allergies and get drowsy, that’s a side effect. The drug worked on your allergies - and it also made you sleepy. That’s built into how the drug works.
The key difference? Preventability. Medication errors can be stopped with better systems. Side effects can’t be avoided entirely - only managed.
How to spot a medication error
Medication errors happen at any step: when a doctor writes the prescription, when the pharmacy fills it, when the nurse gives it, or when you take it at home. Here’s how to recognize them:
- You were prescribed 10 mg, but you got 20 mg.
- You were told to take it with food, but you took it on an empty stomach - and you didn’t know that mattered.
- You got a pill that looks different from last time, and no one explained why.
- You were given a drug that interacts with something else you’re already taking.
- You were given a drug that expired last month.
- You were given a drug meant for someone else.
These aren’t random bad luck. They’re system failures. A 2023 report from the Agency for Healthcare Research and Quality found that 32.7% of all medication errors involve the wrong dose. Another 17.2% involve the wrong strength - especially dangerous for kids. And 22% of IV-related harms come from giving the drug too fast or too slow.
One real case: A patient on vancomycin (an antibiotic) developed kidney damage. The doctor thought it was a side effect. But when they checked the records, the patient’s blood levels hadn’t been monitored for weeks. That’s not a side effect - it’s a medication error. The drug was fine. The monitoring wasn’t.
How to spot a side effect (and why it’s not always bad)
Side effects are predictable. They’re listed on the drug’s label. They happen even when everything is done perfectly. Common ones include:
- Nausea from antibiotics
- Dry mouth from antidepressants
- Weight gain from steroids
- Low blood pressure from blood pressure meds
Here’s the twist: Some side effects are actually useful. Minoxidil was developed as a blood pressure pill. Then doctors noticed patients grew thicker hair. Now it’s a top treatment for baldness. That’s a side effect turned into a benefit.
But not all side effects are harmless. Some can be serious - like liver damage from acetaminophen, or muscle breakdown from statins. The difference? These are still side effects if the drug was given correctly. If the patient took 10 pills instead of 1, that’s an error. If they took 1 as directed and still got liver damage? That’s an adverse drug reaction - a type of side effect that’s more severe and less predictable.
What about adverse drug reactions? Are they the same as side effects?
Yes and no. All side effects are adverse drug reactions - but not all adverse drug reactions are side effects.
The FDA now recommends avoiding the word “side effect” entirely. Why? Because it makes people think it’s harmless. A “side effect” sounds like a minor inconvenience. But an “adverse drug reaction” sounds serious - and it should.
There are two types of adverse drug reactions:
- Type A (80% of cases): Predictable, dose-related. Like dizziness from blood pressure meds. You can often fix this by lowering the dose.
- Type B (15% of cases): Unpredictable, not dose-related. Like a severe allergic reaction to penicillin. These are rare but can be deadly. They’re not your fault - they’re your body’s unpredictable response.
Doctors use the WHO-UMC causality assessment system to decide if a reaction is truly caused by the drug - and whether it’s a Type A or Type B. This matters because Type B reactions need different monitoring and sometimes mean you should never take that drug again.
Why mixing them up puts patients at risk
In a 2023 survey of 8,432 nurses, nearly 70% admitted they weren’t sure how to tell the difference between a medication error and a side effect. And 43% said they’d labeled an error as a side effect to avoid getting in trouble.
That’s a huge problem. If you call a preventable mistake a “side effect,” you’re not fixing the system. You’re just accepting it.
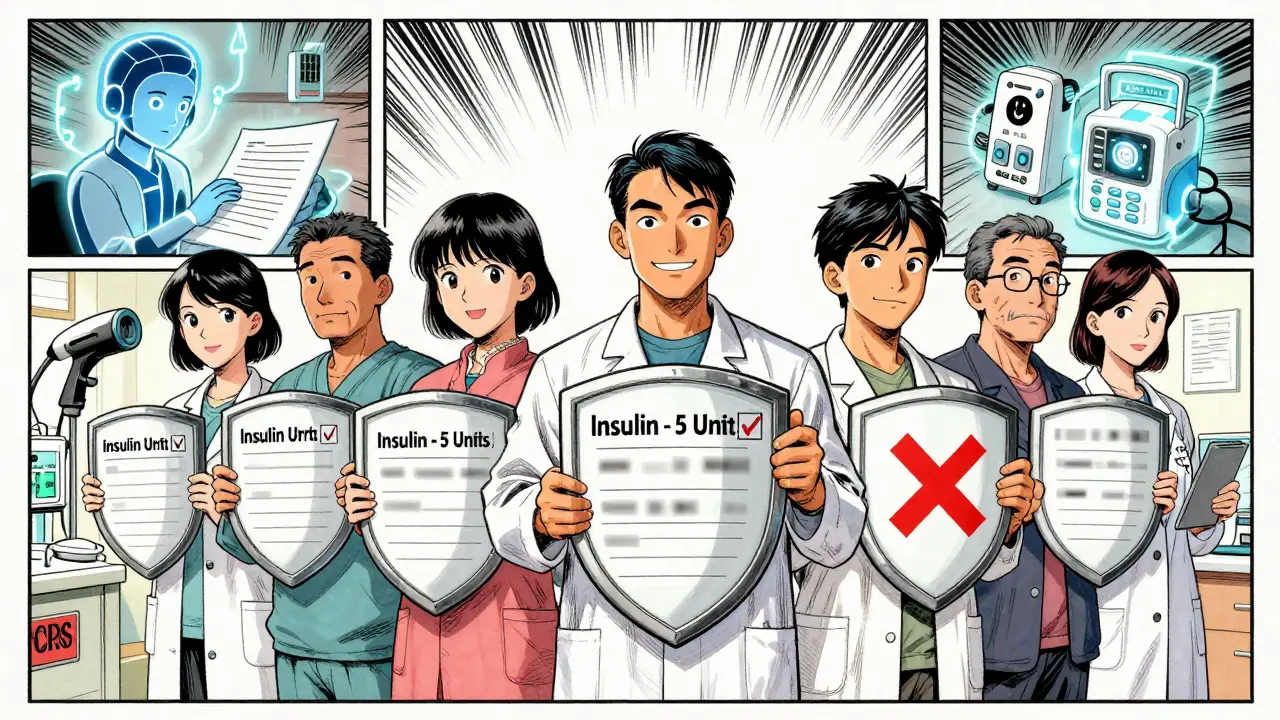
Take this example: A patient in a nursing home gets the wrong dose of insulin because the label was blurry. They go into hypoglycemia. If the staff records this as a “side effect of insulin,” nothing changes. The next person gets the same blurry label. But if it’s recorded as a medication error - a labeling problem - the facility might switch to larger fonts, barcode scanning, or better training. That saves lives.
According to the FDA, 45% of all medication-related harm reports are adverse drug reactions. 32% are medication errors. That means over one-third of injuries are avoidable. But only if we name them right.
What you can do to protect yourself
You don’t need to be a doctor to spot a problem. Here’s how to take control:
- Know your meds. Keep a list of everything you take - including over-the-counter drugs and supplements. Bring it to every appointment.
- Ask questions. “Is this the same pill I got last time?” “What side effects should I watch for?” “What happens if I miss a dose?”
- Check the label. Does the dose match what your doctor said? Is the name correct? Is the expiration date still good?
- Report anything unusual. If you feel worse after starting a new drug, don’t assume it’s “just a side effect.” Call your doctor. Say: “I’m not sure if this is expected or if something went wrong.”
- Use one pharmacy. That way, they can check for dangerous interactions across all your meds.
And if you’re a caregiver for an elderly parent or someone with multiple prescriptions? Be extra careful. Polypharmacy - taking five or more drugs - is the biggest risk factor for errors. One wrong pill can trigger a cascade of problems.
The future is getting smarter - but you still need to be alert
Hospitals are using barcode scanners, computerized prescriptions, and smart IV pumps to cut errors. In 2023, 98% of U.S. hospitals had computerized order systems. But community pharmacies? Only 47%. Nursing homes? 39%.
AI tools are starting to help too. Epic Systems’ new software can scan your medical notes and flag possible errors or reactions with 89% accuracy. But none of this replaces your role as the patient.
Technology reduces errors. It doesn’t eliminate them. And side effects? They’re still going to happen. The goal isn’t to avoid all harm - it’s to know what’s preventable and what’s not.
Bottom line: Know the difference. Speak up.
Medication errors are system failures. Side effects are drug behaviors. One can be fixed. The other can be managed.
If you’re hurt by a drug, ask: “Was this because something went wrong - or because the drug just does this?”
Answering that question correctly could save your life - or someone else’s.


13 Comments
Wow. Just... wow. 🤯 I never realized how much of my anxiety about meds was actually fear of system failures, not the drugs themselves. This post made me check my pill bottle from last week-turns out the label was smudged. I thought it was just me being paranoid. Turns out, I was right to question it. 😅
As a pharmacist for 18 years, I’ve seen this play out too many times. The biggest issue? We’re trained to blame the patient when something goes wrong. ‘Didn’t you read the label?’ No, honey, the label was printed in 6-point font on a sticky note. We need better design, not better patients. And yes-I’ve personally caught 3 wrong-dose errors this month alone. Thank God for barcode scanners.
While the distinction between medication errors and adverse drug reactions is clinically significant, it is equally imperative that healthcare institutions institutionalize standardized reporting protocols. Without consistent taxonomy in documentation, epidemiological tracking becomes unreliable, and systemic improvements remain elusive. This is not merely a patient education issue-it is a structural governance imperative.
Okay, but let’s be real-this whole thing is just a distraction from the fact that Big Pharma doesn’t want you to know how many of these ‘side effects’ are actually just hidden adverse reactions they buried in Phase 3 trials. And don’t get me started on how nurses are pressured to downplay errors to avoid audits. The system is rigged. You think this is about education? It’s about liability. Always has been. And you’re just being manipulated into thinking you’re safe.
You guys are missing the real point. The FDA’s own data shows that 68% of Type B reactions occur in patients over 65 with polypharmacy. That’s not a system failure-that’s biological inevitability. Stop blaming hospitals. Blame aging. Blame genetics. Blame the fact that your grandma’s on 11 meds and her liver is a tired old bus. No amount of barcode scanning fixes that. The real solution? Less meds. Not more tech.
It’s pathetic. People can’t even read a prescription label properly, and now we’re supposed to redesign the entire healthcare system because someone didn’t check their pill bottle? This is why America is falling apart. Take responsibility. Learn your meds. Don’t blame the pharmacist because you’re too lazy to ask questions. My grandmother took 7 drugs daily for 20 years and never had an issue-because she READ THE INSTRUCTIONS.
As someone from India where we get medicines from street vendors and no one checks expiration dates, this post made me cry. We don’t have barcode scanners. We don’t have computerized systems. We have mothers giving their kids the wrong dose because the bottle looks like another one. This isn’t just a US problem-it’s a global crisis. But hey, at least you guys have tech. We just have hope.
OMG YES. I had this happen last month. Took my new blood pressure med, felt dizzy, thought ‘oh, side effect’. Then I checked the bottle-my name was spelled wrong. I had my neighbor’s med. I didn’t even realize until I called the pharmacy. 😳 Now I always double-check the name and dose. And yes, I use one pharmacy. Best life hack ever.
just wanted to say i got the wrong antibiotic once and thought i was allergic. turned out the pill was for someone else. my doc said ‘side effect’ and i believed him. dumb. now i always ask ‘is this the right one?’ and take a pic of the bottle. small things save lives.
THIS IS WHY AMERICA NEEDS MORE MILITARY DISCIPLINE IN HEALTHCARE. NO EXCUSES. NO ‘OH I THOUGHT’. NO ‘SORRY THE LABEL WAS BLURRY’. IF YOU’RE A NURSE, YOU CHECK THE NAME. IF YOU’RE A PHARMACIST, YOU SCAN IT. IF YOU’RE A PATIENT, YOU ASK. NO MORE ‘SIDE EFFECTS’-EVERYTHING IS A FAILURE UNTIL PROVEN OTHERWISE. MAKE AMERICA SAFE AGAIN.
Ugh. I hate when people treat side effects like they’re no big deal. My cousin died from a ‘side effect’ of a statin. It was a Type B reaction. No error. Just bad luck. But now I don’t trust any med. If it’s not essential, I won’t take it. And I tell everyone else the same. Don’t be fooled by pretty labels.
To everyone who’s been scared or confused by meds-please know you’re not alone. And you’re not failing. The system is the one that needs fixing. But you? You’re already doing better than most by reading this, asking questions, and caring enough to learn. That’s courage. That’s power. Keep going. One pill, one question, one label at a time-you’re changing the game. 💪❤️
Just wanted to say thank you for writing this. I’m a caregiver for my mom, and I used to just nod along when the doctor said ‘side effect.’ Now I ask: ‘Is this preventable?’ If yes-I push. If no-I help her manage it. You made me feel like I’m not just a helper. I’m part of the solution. 🫶
Write a comment