More than 14 million people travel abroad each year for medical care. They’re going to Thailand for knee replacements, Mexico for dental work, Turkey for hair transplants, and South Korea for cutting-edge cancer treatments. The savings are real - sometimes 60% or more off U.S. prices. But behind the deals and glossy brochures, there’s a quiet danger most travelers don’t think about until it’s too late: medication safety.
Why Medication Safety Is the Hidden Risk in Medical Tourism
You wouldn’t buy a fake iPhone and expect it to work safely. Yet every year, people travel overseas, get prescribed medications, and come home with pills that don’t match what they were told - or worse, aren’t what they claim to be. The World Health Organization estimates that 1 in 10 medical products in low- and middle-income countries are substandard or falsified. That means fake antibiotics, diluted painkillers, or pills with no active ingredient at all. Even in countries with stronger systems like Turkey or Thailand, differences in drug approval standards mean a medication you get abroad might not be legal - or even available - back home. Take a patient who gets a heart stent in India. They’re sent home with a blood thinner called clopidogrel. Back in the U.S., their doctor tries to refill it - but the brand they received isn’t sold here. The generic version works differently. The dosage is off. The patient ends up in the ER with a clot. This isn’t rare. DelveInsight reports that 26% of medical tourists face follow-up care problems, and medication mismanagement is one of the top causes.How Drug Regulations Vary Around the World
Every country has its own rules for what drugs can be sold, how they’re made, and who can prescribe them. The U.S. FDA has strict testing and manufacturing standards. The European Union has similar rules. But in many popular medical tourism destinations, those standards are either weaker or inconsistently enforced. For example:- In Mexico, some clinics use antibiotics not approved by the FDA, like ciprofloxacin in higher doses than allowed in the U.S.
- In India, generic drugs are common and affordable - but not all generics are bioequivalent. One study found some Indian-made versions of antiretrovirals had up to 30% less active ingredient.
- In Thailand, JCI-accredited hospitals follow international standards, but smaller clinics don’t. A patient might get a prescription from a hospital that meets global standards, then pick up their meds from a local pharmacy that doesn’t.
- In South Korea, new cancer drugs are approved faster than in the U.S. - but those same drugs might be experimental or untested in other populations.
What Happens When You Get Home
The biggest problem isn’t just what you get abroad - it’s what happens after you return. Most patients don’t bring their full medical records. They don’t have a list of every drug they were given, including dosages and expiration dates. Their home doctor doesn’t know what they took, why they took it, or if it’s still safe to use. Imagine this: You get a hip replacement in Malaysia. You’re sent home with a strong painkiller, an antibiotic, and a blood thinner. You don’t write down the names. You don’t know the generic equivalents. You get home, your regular doctor sees you - and says, “We don’t prescribe that painkiller here.” Now you’re in pain. You can’t refill the antibiotic. You stop the blood thinner because you’re scared of side effects - and risk a clot. This isn’t hypothetical. A 2024 study of 500 returning medical tourists found that 43% couldn’t identify even one medication they were prescribed abroad. Nearly 30% had to restart treatment because their home pharmacy couldn’t fill the prescription.
What You Can Do to Protect Yourself
You don’t have to avoid medical tourism. But you do need to treat medication safety like you’d treat travel insurance - something you plan for before you leave. Before you go:- Ask your home doctor to review your planned procedure and any medications you’ll likely need. Get their input on what’s safe and what alternatives exist.
- Confirm the hospital or clinic is accredited by JCI or another recognized body. Accreditation doesn’t guarantee perfect medication safety - but it’s a strong signal they follow international standards.
- Ask for a full list of all medications you’ll receive - brand name, generic name, dosage, frequency, and purpose. Get it in writing.
- Take photos of your prescriptions and pill bottles. Don’t rely on memory.
- Find out if the medications you’re getting are approved in your home country. Search the FDA, Health Canada, or your national drug agency’s website.
- Don’t accept medications from street pharmacies or unlicensed vendors. Even if they’re cheaper, they’re not worth the risk.
- Ask if the pharmacy is licensed and if the drugs come from a registered distributor. Most reputable clinics will let you see the pharmacy’s license.
- Keep all packaging, labels, and receipts. You’ll need them later.
- Bring your full medical records and medication list to your primary care provider within 48 hours of returning.
- Don’t assume your home doctor knows what you were given. Bring printed lists, photos, and bottles.
- Ask your doctor to check for interactions with your existing meds. Many patients are on multiple drugs - and a new one can cause serious side effects.
- If you can’t refill a medication, ask your doctor for a safe substitute - don’t skip doses or guess.
The Rise of Digital Health - And Its Limits
Some clinics now offer digital health records and telemedicine follow-ups. South Korea’s Severance Hospital, for example, uses AI to track genetic responses to cancer drugs and shares data with international patients. That’s a step forward. But here’s the catch: Not every clinic does this. And even when they do, your home doctor may not have access to the same system. A digital record from a hospital in Bangkok won’t automatically sync with your U.S. electronic health record. You still have to carry the information yourself. Telemedicine follow-ups help - but only if you’re connected to a provider who understands your home country’s drug standards. A chat with a nurse in Manila won’t help if your doctor in Chicago doesn’t know what drug you were given.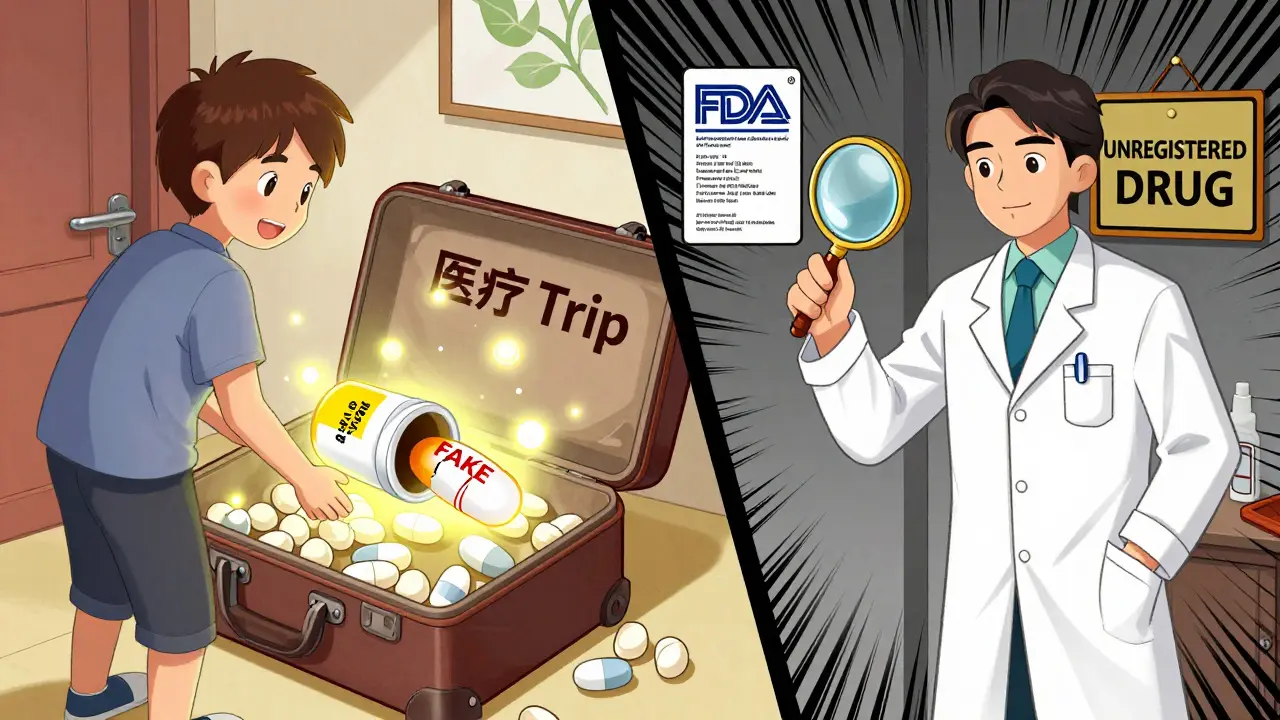
Wellness Tourism Adds Another Layer of Risk
Medical tourism isn’t just about surgery anymore. It’s also about wellness: stem cell therapies, IV vitamin drips, anti-aging hormones, and unregulated supplements. Many of these aren’t drugs at all - they’re marketed as “nutritional support” or “regenerative treatments.” But they often contain active ingredients that aren’t approved anywhere. Some contain steroids, hormones, or heavy metals. Others are just saline water in fancy bottles. A 2025 report from the International Healthcare Research Center found that 1 in 5 wellness tourists received injections or oral treatments containing unapproved substances. In some cases, those substances caused liver damage, hormonal imbalances, or allergic reactions. If you’re going for a “detox” or “longevity treatment,” ask: Is this FDA-approved? Is it legal in my country? Who tested it? If the answer is “it’s natural” or “everyone uses it,” walk away.Who’s Responsible When Something Goes Wrong?
This is the hardest question - and no one wants to talk about it. If you get a bad drug abroad, who pays for your ER visit? Who covers your lost wages? Who’s liable if you have a stroke because a fake blood thinner didn’t work? Most medical tourism packages don’t include insurance for medication errors. Travel insurance usually covers accidents, not bad prescriptions. Your home health plan won’t touch it. You’re on your own. Some countries have started creating legal pathways. Thailand has a medical tourism ombudsman. India has a registry of approved clinics. But enforcement is patchy. And if you’re from the U.S., Canada, or the U.K., you’re still outside the legal system of the country where you were treated.Final Thought: Savings Shouldn’t Cost You Your Health
Medical tourism can be smart. It can save you thousands. It can give you access to treatments you couldn’t get at home. But those savings mean nothing if you come back sicker than when you left. Medication safety isn’t a side note. It’s the core risk. And it’s one you can control - if you plan for it. Don’t just pick a destination because it’s cheap. Pick one that’s transparent. Ask for proof. Demand details. Keep records. Talk to your doctor - before you book your flight. The best medical tourism isn’t the one with the lowest price. It’s the one where you know exactly what you’re taking - and why.Are medications from medical tourism destinations safe?
Some are, some aren’t. Countries with strong regulations - like Thailand, Turkey, and South Korea - often use approved medications in accredited hospitals. But in places with weaker oversight, up to 1 in 10 drugs may be substandard or fake. Always ask for the drug’s name, manufacturer, and approval status. Never take medication from unlicensed pharmacies.
Can I refill my foreign-prescribed medication in my home country?
Not always. Many drugs prescribed abroad aren’t available or approved in your home country. Even if they are, the brand, dosage, or formulation might differ. Always bring a full list of your medications and ask your doctor for a safe, approved alternative before you leave.
What should I do if I can’t identify a medication I was given abroad?
Take photos of the pills and packaging, and bring them to your doctor immediately. Use a pill identifier app like WebMD’s or Drugs.com as a starting point - but don’t rely on it alone. Your doctor may need to order blood tests to check for drug levels or side effects. Never guess what a pill is.
Is JCI accreditation enough to ensure medication safety?
JCI accreditation ensures high standards for facilities, staff, and infection control - but it doesn’t guarantee perfect medication safety. Some JCI hospitals still use drugs not approved in your home country. Always ask what medications you’ll receive and verify them with your own doctor before leaving.
Should I avoid medical tourism because of medication risks?
No - but you should approach it like a high-stakes decision. The risks are real, but they’re manageable. Do your research, ask tough questions, bring your own records, and work with your home doctor before and after. Medical tourism can be safe - if you treat medication safety as seriously as you treat the surgery itself.


15 Comments
Fake meds are a global problem but calling out India specifically is lazy. Most generics are fine. The real issue is unregulated clinics, not the drugs themselves.
This is so important 😰 I went to Mexico for dental work and got a pill that looked like a candy. I still have the bottle. Don't trust anything without a barcode.
The WHO's 1-in-10 statistic is misleadingly aggregated. Substandard pharmaceuticals in low-income countries are not equivalent to falsified drugs in JCI-accredited Thai hospitals. The risk profile is not uniform across geographies or institutions. One must disaggregate data before drawing behavioral conclusions.
I had a knee replacement in Thailand. Got the meds from the hospital pharmacy, not a street vendor. Took pics of every bottle. Brought the list to my doctor. No issues. It’s not about avoiding travel-it’s about being smart.
I love how this post doesn't just scare people-it gives you a clear action plan. Before you go, talk to your doctor. While you're there, ask for paperwork. When you come back, bring the bottles. Simple. Effective.
USA thinks its FDA is god but they block life saving drugs for profit. India and Thailand give real medicine cheap. You Americans are so paranoid you die from overthinking. The truth is you just dont want poor people to get better
Medication safety is just one layer of the existential crisis of modern healthcare capitalism. When your body becomes a commodity and your pain a market segment, the pills you get are just symbols of a deeper collapse
In India, some generics are good some are not. But if you go to a hospital with NABH cert, you are fine. Dont listen to fear. Do your homework. I did. Got my stent. No problem.
Oh wow, so now we’re supposed to be terrified of every pill from abroad? I got my insulin in Mexico for $12. My US doctor couldn’t even give me a refill without a 3-month wait. Who’s the real villain here?
I went to Turkey for a hair transplant and got a cream with no label. I panicked and took a photo. Turned out it was just aloe vera with a weird brand. But I still showed it to my dermatologist. Better safe than sorry!
The notion that Western pharmaceutical regulation is superior is colonial arrogance. India produces 40% of the world's generic drugs. To suggest their quality is suspect is not only inaccurate-it is offensive to millions who rely on these medicines daily.
I think the real takeaway is that we need better global coordination. Why can't a pill from India be in the FDA database? Why can't hospitals share records across borders? It's not about fear-it's about infrastructure
Wait-so if I get a drug in South Korea that’s not approved in the US, does that mean it’s experimental? Or just not marketed here? I’m confused. Is there a public database where I can check this?
There’s a quiet dignity in taking responsibility for your own health. No one else will do it for you. The fact that you’re reading this means you’re already ahead of most. Keep asking questions. Keep documenting. Keep trusting your own curiosity.
The pharmacovigilance gap between JCI-accredited institutions and peripheral pharmacies is not a flaw-it is a structural vulnerability in the global supply chain. Bioequivalence studies are often underpowered in LMICs, and therapeutic substitution without clinical correlation is a latent iatrogenic hazard. Document, verify, escalate.
Write a comment