Every year, thousands of people end up in emergency rooms because of drug reactions that could have been avoided. Not because the medicine was wrong - but because the right information wasn’t written down clearly in their medical records. If you’ve ever said, "I’m allergic to penicillin," without explaining what happened, you might be putting yourself at risk. The truth is, most people don’t know how to document their drug allergies properly - and neither do many doctors. But getting this right isn’t just helpful. It’s life-saving.
Why Vague Allergy Notes Are Dangerous
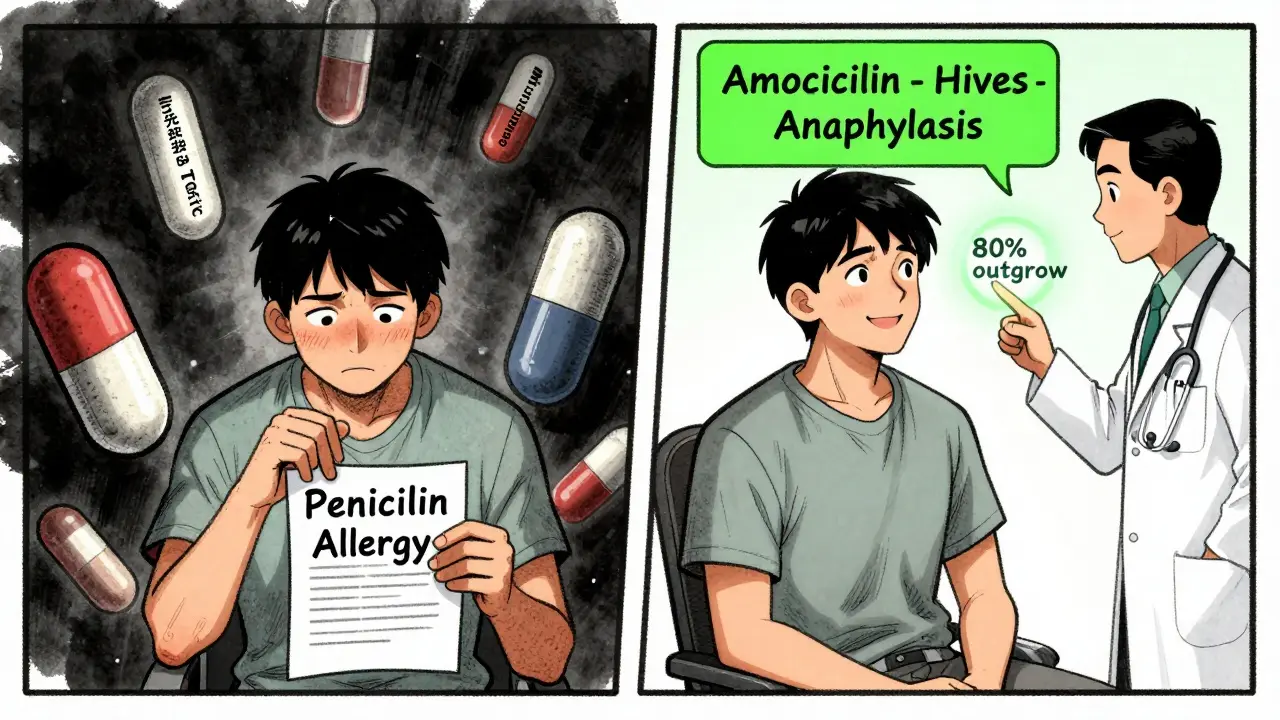
When you tell your doctor, "I had a rash after taking sulfa," that’s not enough. What kind of rash? Did you swell up? Could you breathe? Did it happen hours later or days after? If the record just says "sulfa allergy," your next doctor might avoid every sulfa-based drug - even ones that are safe for you. And that’s a problem. Many antibiotics in the sulfa family are the only effective treatment for certain infections. Avoiding them unnecessarily means you might get a less effective, more expensive, or more toxic drug instead. A 2018 study at Massachusetts General Hospital found that over 60% of patients needed their allergy records changed after a simple 10-minute interview. Nearly 200 vague entries like "allergic to penicillin" were clarified. Many turned out to be side effects - not true allergies. That’s because 90% of people who think they’re allergic to penicillin aren’t. Without clear documentation, you’re stuck with that label forever.What Exactly Needs to Be Documented
The U.S. government doesn’t leave this to chance. Medicare and Medicaid require every medical record to include three things for any drug allergy:- The exact generic name of the drug (e.g., ampicillin, not penicillin or antibiotic)
- The specific reaction you had (e.g., hives, swelling, trouble breathing, anaphylaxis)
- The severity and timing (e.g., "Severe anaphylaxis 15 minutes after first dose")
How to Tell Your Doctor the Right Way
Don’t wait for your doctor to ask. Bring this info with you to every appointment - especially before surgery or hospital visits. Here’s how to make it clear:- Start with the drug name: "I had a reaction to amoxicillin," not "penicillin."
- Describe the reaction: "My face swelled up, my throat closed, and I couldn’t breathe."
- Include timing: "It happened within 20 minutes of taking the pill."
- State the severity: "I needed epinephrine and went to the ER."
What’s Not an Allergy - And Why It Matters
Many people confuse side effects with true allergies. Here’s the difference:- True allergy: Your immune system reacts. Symptoms: hives, swelling, wheezing, anaphylaxis, low blood pressure. These are dangerous and can be life-threatening.
- Intolerance or side effect: Your body doesn’t handle the drug well. Symptoms: nausea, headache, diarrhea, dizziness. These are unpleasant, but not immune-driven. You can often try the drug again, or a similar one, safely.
How EHRs Are Changing the Game
Most clinics now use electronic health records (EHRs) like Epic or Cerner. These systems have built-in tools to help. When you type in a drug name, the system should pop up a box asking: "What reaction did you have?" If it doesn’t - ask your provider to use it. Good EHRs also:- Require you to pick a reaction type from a list - not just type free text
- Flag high-risk allergies in bright red at the top of your chart
- Block prescriptions if a dangerous drug is ordered for you
What to Do If Your Records Are Wrong
If you’ve been labeled allergic to a drug you’re not - or if your record is missing key details - you can fix it. Here’s how:- Request a copy of your medical records. You have the legal right to them.
- Review every allergy listed. Are they specific? Are they accurate?
- If something’s vague or wrong, ask your primary care doctor to review it.
- Ask for a referral to an allergist. Skin or blood tests can confirm if you’re truly allergic.
- Once you have proof, ask your doctor to update your record - and get it in writing.
What’s Next: Patient Tools and AI
New tools are making this easier. The FDA is testing apps like MyStudies that let you log drug reactions on your phone. Your doctor can pull that data into your record later. In 2025, all EHRs will be required to include patient-facing allergy tools so you can update your own info securely. AI is also helping. One study found that algorithms could read doctor’s notes and pull out allergy details with 86% accuracy - but only if the notes were detailed enough. That means your clear, specific description today helps AI help you tomorrow.Final Checklist: Your Drug Allergy Record
Before your next appointment, check this list:- Are all drug names written as generic names? (e.g., ibuprofen, not Advil)
- Is each reaction described in detail? (e.g., hives, swelling, breathing trouble)
- Is severity and timing noted? (e.g., "Severe, within 10 minutes of taking it")
- Is there a clear "No Known Allergies" note if applicable?
- Have you reviewed this list in the last 12 months?
What if I don’t remember which drug caused my reaction?
It’s okay not to know the exact drug. Write down what you do remember: the symptoms, when it happened, and what the medicine was for (e.g., "I got sick after taking a pill for a sinus infection in 2020"). Your doctor can look up what drugs are typically prescribed for that condition and help narrow it down. Never guess - just be honest about what you’re unsure of.
Can I outgrow a drug allergy?
Yes, especially with penicillin. Studies show that 80% of people who had a penicillin allergy as a child lose it within 10 years. But unless you get tested, your record will still say you’re allergic. If you haven’t had a reaction in over a decade, ask your doctor about an allergy test. It’s a simple skin prick or blood test - and it could open up safer treatment options.
Does my pharmacist see my allergy record?
If your pharmacy is connected to the same electronic system as your doctor’s office - yes. But not always. Some independent pharmacies still use separate systems. Always tell your pharmacist about your allergies when picking up a new prescription. Don’t assume they already know. Your record might be perfect, but the system might not have shared it.
What if I have a reaction to a new drug? Should I update my record right away?
Yes - and immediately. Even if it seems mild. Write down the drug name, what happened, and when. Then call your doctor. Don’t wait for your next appointment. A reaction that seems like a rash today could be a warning sign of something worse next time. Getting it documented now protects you in the future.
Are food allergies and drug allergies documented the same way?
No. Food allergies are usually documented separately, often under "Allergies" or "Immunology." Drug allergies go under "Medication Allergies" or "Drug Reactions" in your medical record. Make sure both are clearly labeled. If you’re allergic to peanuts and penicillin, don’t just write "allergic to peanuts and penicillin." List them separately with details for each.


15 Comments
Just updated my EHR after reading this. Used to say 'allergic to penicillin' - now it says 'hives + swelling 15 min after amoxicillin, 2018, required epinephrine'. Feels good to actually be accurate instead of just lazy.
Thanks for the checklist. I'm printing this.
they're all lying about penicillin anyway. the government made up allergies so they could sell you more expensive drugs. i got the rash from the dye in the pill. not the medicine. they don't want you to know that.
It’s refreshing to see someone articulate the distinction between immune-mediated hypersensitivity and pharmacological intolerance with such precision. The fact that 90% of penicillin 'allergies' are mislabeled is not just a clinical oversight-it’s a systemic failure of documentation culture.
Oh wow, so now we’re supposed to become amateur allergists just so the EHR doesn’t glitch? Brilliant. Let’s just add ‘I think I might’ve been allergic to something once, but I’m not sure, but my doctor wrote it down anyway’ to the DSM-5.
This is the kind of post that makes me believe in humanity again. Seriously. We’re talking about real people getting better care because someone took five minutes to write down what actually happened.
And yes, if you got diarrhea from amoxicillin - you’re not allergic. You’re just a human with a gut. But if your throat closed? That’s a red flag. Not a suggestion.
Update your records. It’s not bureaucracy. It’s self-preservation.
And if you’re scared to ask your doctor? Bring this article. They’ll thank you.
Curious - do EHR systems differentiate between IgE-mediated reactions and T-cell mediated ones? I’ve seen cases where a rash from vancomycin (red man syndrome) gets misclassified as an allergy, even though it’s a pharmacological reaction.
Let’s be real - most clinicians don’t care. They copy-paste 'penicillin allergy' from the last visit. The FHIR standard is a joke if the front desk still types 'allergic to antibiotics' in the notes. This is a band-aid on a hemorrhage.
so i had a rash after penicillin in 1999
now i can't take any abx
but i'm fine with cipro
but the system says i'm allergic to all
so i just say no allergies
and hope for the best
lol
It is, however, profoundly concerning that the onus of medical accuracy is being placed upon the patient - a layperson - rather than the healthcare infrastructure that has, for decades, failed to implement standardized, interoperable, and intelligently structured allergy documentation protocols. One cannot help but wonder: who is really responsible for this failure?
I was terrified to ask for a skin test because I thought they’d think I was crazy…
But I did it. Turns out I’m not allergic to penicillin. I’ve been on amoxicillin three times since. No problem.
My doctor cried. I cried.
It’s not just about drugs. It’s about freedom.
Oh please. You think your 'detailed allergy' matters? My cousin got misdiagnosed because the system auto-filled 'penicillin allergy' from a 1987 chart. They gave him clindamycin instead. He got C. diff and lost his colon. So yeah - your 'accurate notes' are just noise in a broken machine.
In my village in rural India, we don’t have EHRs. We have a notebook. My aunt wrote: 'Penicillin - face swelled, hospital, saved by shot'. No fancy terms. Just truth.
Maybe the answer isn’t more tech. Maybe it’s just… remembering to write it down.
Simple. Human.
As a former hospital administrator, I can confirm: the CMS requirements are technically enforced - but in practice, the documentation is often incomplete because the EHR interface is designed by engineers who have never held a stethoscope.
And yet, we still penalize providers for 'non-compliance'.
It’s not the patient’s fault. It’s the system’s.
You got this 💪
Update your records. Bring this to your next visit. Tell your mom. Tell your bestie.
One clear note could save your life… or someone else’s.
And if you're scared? Just say: 'I want to make sure I'm not being unnecessarily limited.'
They’ll respect you for it. 😊
Interesting. In India, we often rely on family memory. My grandfather had a reaction to streptomycin in the 1970s - now my whole family avoids it. No documentation. Just tradition. But this article made me realize - maybe we should start writing it down. Even if it’s just on a phone note.
Write a comment