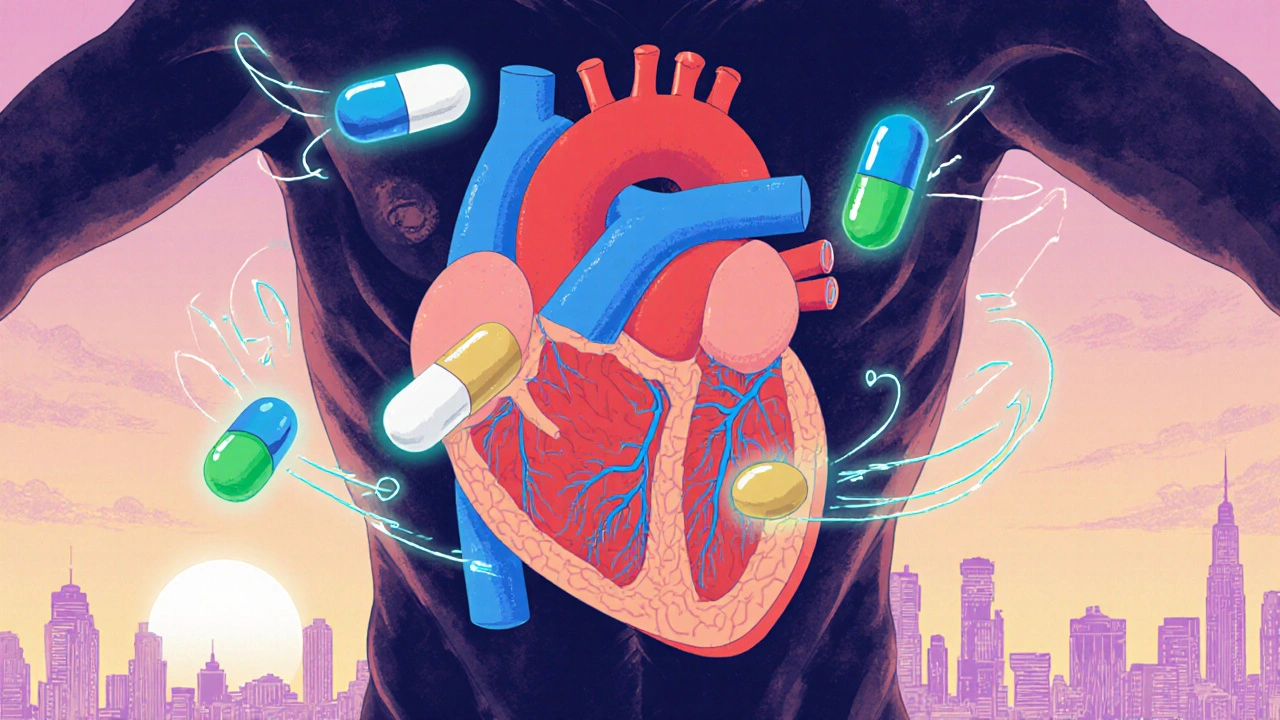
When you’re diagnosed with heart failure, especially with reduced ejection fraction (HFrEF), the right medications can mean the difference between struggling to breathe and living well. Four drug classes form the backbone of modern treatment: ACE inhibitors, ARNI, beta blockers, and diuretics. These aren’t just pills on a list-they’re tools that change how your heart works, how much fluid builds up in your body, and how long you live.
ACE Inhibitors: The First Line for Decades
ACE inhibitors like enalapril, lisinopril, and ramipril have been around since the 1980s. They work by blocking the enzyme that turns angiotensin I into angiotensin II-a hormone that tightens blood vessels and forces the heart to work harder. By stopping this, ACE inhibitors lower blood pressure, reduce strain on the heart, and slow down damage.The CONSENSUS trial in 1987 showed enalapril cut death rates by 27% in people with severe heart failure. That was a game-changer. Today, these drugs are still used, but they’re no longer the first choice for new patients. Why? Because something better came along.
Side effects are common. About 1 in 5 people get a dry, annoying cough. Some develop high potassium levels (hyperkalemia), which can be dangerous if not caught. Rarely, swelling of the face or throat (angioedema) happens-this needs emergency care. If you can’t tolerate an ACE inhibitor, you’re not alone. About 10-15% of patients switch to something else.
ARNI: The New Standard That Replaced ACE Inhibitors
Sacubitril/valsartan (brand name Entresto) is the biggest leap in heart failure treatment since beta blockers. Approved by the FDA in 2015, it’s not just another drug-it’s a combo. Sacubitril blocks neprilysin, which lets natural heart-protecting peptides like natriuretic hormones work better. Valsartan blocks angiotensin receptors, like an ARB. Together, they do more than ACE inhibitors ever could.The PARADIGM-HF trial tracked nearly 8,400 people across 47 countries. Those on Entresto had 20% fewer deaths from heart problems and 21% fewer hospital stays than those on enalapril. That’s not a small win-it’s life-changing.
But there’s a catch. You can’t start Entresto if you’ve taken an ACE inhibitor in the last 36 hours. The risk of angioedema jumps. Doctors will make you wait. Also, Entresto costs about $550 a month without insurance. Many patients can’t afford it, and insurance often requires prior authorization.
Still, adoption is rising. In 2023, 62% of newly diagnosed heart failure patients got ARNI as their first drug, up from just 28% in 2018. In academic hospitals, it’s over 65%. In small clinics? Only 42%. Cost and familiarity are the biggest barriers.
Beta Blockers: Slowing Down to Save the Heart
It sounds backwards-why slow down a heart that’s already struggling? But in heart failure, the heart is overworked and burning out. Beta blockers like carvedilol, metoprolol succinate, and bisoprolol calm the nervous system, reduce heart rate, and lower blood pressure. They don’t fix the problem right away-they give the heart time to heal.The CIBIS-II trial showed bisoprolol cut death risk by 34%. The COPERNICUS trial found carvedilol lowered death risk by 35% in severe cases. These aren’t just numbers-they’re real lives saved.
But starting them is tricky. You begin at a tiny dose: 3.125 mg of carvedilol twice a day, or 12.5 mg of metoprolol once daily. You wait two to four weeks before doubling it. If your blood pressure drops too low or you feel dizzy, you hold off. Many patients get tired, sluggish, or have a slow pulse. Some quit because they feel worse at first.
But here’s what patients say on forums like Reddit: u/CHFSurvivor shared their ejection fraction jumped from 25% to 45% after 18 months on carvedilol. That’s not luck-it’s science. The benefits come slowly, but they last.
Diuretics: Managing the Swelling
Diuretics don’t extend life. But they make life bearable. When your heart fails, fluid backs up into your lungs, legs, and belly. You feel bloated, short of breath, and heavy. Diuretics flush that out.Loop diuretics like furosemide, bumetanide, and torsemide are the go-to. Furosemide is the most common-starting at 20-80 mg daily, adjusted until swelling goes down. Torsemide may be better: the EVEREST trial showed it led to 18% fewer hospitalizations than furosemide.
Thiazides like hydrochlorothiazide are weaker but used for mild cases or with other diuretics. Spironolactone is special-it’s both a diuretic and a mineralocorticoid receptor antagonist (MRA). It reduces death by 30% in the RALES trial, but it raises potassium. Many patients need regular blood tests to watch for that.
Side effects? Frequent urination, dehydration, leg cramps, and low sodium. Some patients take potassium or magnesium supplements to fight cramps. u/HeartWarrior2020 on PatientsLikeMe said cramps vanished after adding magnesium. Simple fixes, big relief.
How These Drugs Work Together
The current standard isn’t one drug-it’s four. The 2022 AHA/ACC/HFSA guidelines call this quadruple therapy:- ARNI (instead of ACEI or ARB)
- Beta blocker
- Mineralocorticoid receptor antagonist (like spironolactone)
- SGLT2 inhibitor (like dapagliflozin or empagliflozin)
Diuretics are added on top if you’re still swollen. This combo reduces death by up to 20% and hospitalizations by 21%. But here’s the hard truth: only 35% of eligible patients get all four within a year of diagnosis.
Why? Because titrating these drugs is hard. It takes time, patience, and frequent follow-ups. Many doctors don’t have the resources. Patients get overwhelmed. One patient told me, “I had to see three specialists just to get my doses right.”
Heart failure clinics with nurses, pharmacists, and care coordinators get 85% adherence. Regular clinics? Only 52%. If you’re getting care at a hospital with a dedicated heart failure team, you’re more likely to survive and thrive.
What to Watch For
These drugs are powerful, but they need monitoring:- Potassium: Keep it under 5.0 mmol/L. Too high can cause dangerous heart rhythms.
- Creatinine: A 30% rise from baseline means your kidneys are stressed. Dose adjustments may be needed.
- Blood pressure: You need at least 100 mmHg systolic to safely start or increase ARNI or beta blockers.
- Heart rate: Don’t increase beta blockers if your resting heart rate is below 50 bpm.
Get blood tests 1-2 weeks after starting or changing any of these drugs. An echocardiogram at 3-6 months shows if your heart is improving. Many patients don’t know this-they think if they feel better, they’re fine. But your heart might still be weakening underneath.
Real Patient Stories
On Amazon, heart failure meds average 4.1/5 stars. Diuretics get high marks for symptom relief but low ones for frequent bathroom trips. Beta blockers get 3.7/5-people appreciate the long-term benefit but hate the fatigue. ARNI gets the highest rating: 4.3/5.u/PumpFailure on Reddit switched from lisinopril to Entresto and noticed less shortness of breath in two weeks. But they started peeing more often-so much they had to plan their day around bathrooms.
Another user, u/HeartWarrior2020, had terrible leg cramps from furosemide. After adding magnesium, they disappeared. Simple fix. Big difference.
These aren’t just case studies. They’re real people managing a chronic disease with a mix of science, trial and error, and persistence.
What’s Next?
The future is expanding. In 2023, the FDA approved ARNI for heart failure with mildly reduced ejection fraction (HFmrEF)-adding millions more people who can benefit. SGLT2 inhibitors, originally for diabetes, are now recommended for all heart failure types, even if ejection fraction is normal.Drugs like vericiguat (for advanced cases) are being added to the mix. But the biggest challenge isn’t new drugs-it’s access. In rural areas, only 28% of eligible patients get guideline-recommended therapy. Cost, lack of specialists, and poor follow-up keep people from getting the care they need.
By 2027, experts predict ARNI will be first-line for 70% of HFrEF patients. But until we fix the system-until insurance covers these drugs without endless paperwork, until clinics have the staff to titrate doses properly, until patients get educated and supported-we’re still leaving too many behind.
Can I take ACE inhibitors and ARNI together?
No. You must wait at least 36 hours after your last ACE inhibitor dose before starting ARNI. Taking them together increases the risk of angioedema-a dangerous swelling of the face, lips, or throat. This is a strict safety rule backed by clinical trials and the FDA.
Why do beta blockers make me feel so tired?
Beta blockers slow your heart rate and reduce the force of your heartbeat. That lowers blood pressure and protects your heart over time-but it also reduces energy. Fatigue is common in the first few weeks. Most people adapt within 4-8 weeks. If you’re still exhausted after two months, talk to your doctor about adjusting the dose. Never stop cold turkey-it can trigger dangerous heart rhythms.
Is ARNI better than ACE inhibitors?
Yes, for most people with heart failure and reduced ejection fraction. The PARADIGM-HF trial showed ARNI reduced death and hospitalization by 20% compared to enalapril. It’s now the recommended first-line therapy. If you’re already on an ACE inhibitor and doing well, switching isn’t always necessary-but if you’re newly diagnosed, ARNI should be your starting point, unless you can’t afford it or have contraindications.
Do diuretics help you live longer?
Not directly. Diuretics don’t reduce death rates like ARNI or beta blockers do. But they’re essential for quality of life. Without them, fluid builds up, making it hard to breathe, walk, or sleep. Many patients say diuretics let them live at all. Torsemide may be better than furosemide at preventing hospitalizations. Always use the lowest effective dose to avoid dehydration and electrolyte imbalances.
How long does it take for heart failure meds to work?
Diuretics work in hours or days-you’ll notice less swelling and easier breathing. Beta blockers and ARNI take weeks to months. You might feel worse at first as your body adjusts. Don’t give up. Improvements in energy, walking distance, and hospital visits show up over 3-6 months. Your ejection fraction may improve too-some patients see gains of 10-20% after a year on the right combo.
What to Do Next
If you’re on heart failure meds:- Keep a log: Note your weight daily, symptoms, and side effects.
- Ask for a referral to a heart failure clinic if you’re not in one.
- Request a blood test 1-2 weeks after starting or changing any drug.
- Don’t skip doses because you feel better-these drugs work over time.
- If cost is an issue, ask about patient assistance programs. Novartis offers help for Entresto.
Heart failure is serious, but it’s not a death sentence. With the right meds, monitored carefully, many people live for years with good quality of life. The science is clear. The challenge now is making sure everyone gets access to it.

8 Comments
Look, I get it-ARNI is the new hotness, but let’s be real: most docs still prescribe lisinopril because it’s cheap, familiar, and their EHR auto-fills it. I’ve been on it for 5 years and I’m fine. Why should I switch just because some trial says so? My blood pressure’s stable, I don’t cough, and I’m not broke. This ‘gold standard’ nonsense is just pharma pushing their $550/month miracle pill while I’m choosing between insulin and my meds. 🤷♂️
It’s fascinating how medicine has evolved from treating symptoms to reshaping biology. ACE inhibitors were a breakthrough because they addressed the neurohormonal cascade-something we didn’t even know existed in the 80s. Now ARNI doesn’t just block a pathway; it enhances protective peptides. It’s not just pharmacology-it’s a philosophical shift from suppression to restoration. But I wonder… if we’re so focused on drugs, are we neglecting the root causes? Diet, stress, sleep, inflammation? The heart doesn’t fail because of angiotensin-it fails because we’ve forgotten how to live.
Diuretics saved my dad’s life. He couldn’t walk 10 steps without gasping. After starting torsemide, he slept through the night for the first time in years. No magic pill-but a simple one. Also, magnesium helped his cramps. Simple, cheap, real.
Let’s cut through the BS. ARNI isn’t better-it’s a rebranded combo designed to bypass patent cliffs. The PARADIGM-HF trial? Funded by Novartis. The ‘20% reduction’? Statistically significant but clinically marginal for many. And don’t get me started on SGLT2 inhibitors being shoved into heart failure like a diabetic afterthought. This is profit-driven medicine disguised as science. They’re selling a regimen, not a cure. You think your doctor cares about your ejection fraction? They care about their QI metrics and HEDIS scores. You’re a data point with a pulse.
Bro I was on carvedilol for 6 months and felt like a zombie 😴 I thought I was dying but my cardiologist said ‘it’s the meds adjusting’-and holy smokes after 3 months I could climb stairs without panting. My EF went from 28% to 42%! 🙌 Also, if you’re on ARNI, DO NOT take ACEi in the last 36hrs-angioedema ain’t a joke, I saw a guy get intubated at the ER. Also, if you’re poor, ask for Novartis patient help-they got a program, I got my Entresto for $5/mo 💪❤️
I just want to say thank you to everyone who shared their stories. I was diagnosed last year and felt so alone. Reading about people getting their energy back, their cramps gone, their breathing easier-it gave me hope. I’m not ‘fixed,’ but I’m not giving up either. Small wins matter. You’re not just numbers on a trial. You’re real. And you’re not alone.
Oh for fuck’s sake, another 3,000-word medical manifesto. I came here for a quick read, not a damn textbook. Can we just agree that diuretics make you pee like a racehorse and beta blockers turn you into a sloth? ARNI’s fancy, sure-but if I can’t afford it, it’s just a luxury sedan in a parking lot with no gas. And don’t even get me started on ‘quadruple therapy’-I’ve got four prescriptions already, a pill organizer bigger than my laptop, and a nurse who calls me ‘honey.’ I’m not a protocol. I’m a man trying not to die. Can we simplify this shit?
I’ve been managing HFrEF for eight years now, and the biggest takeaway isn’t the drug class-it’s the system. I live in rural Australia, and getting a blood test took three weeks. My GP didn’t know the difference between spironolactone and eplerenone. I had to fly to Brisbane to see a heart failure clinic, and even then, I waited six months. The science is brilliant-ARNI, SGLT2i, beta blockers, MRAs-it’s a symphony. But the delivery? A broken metronome. We need decentralized care: nurse practitioners trained in heart failure, telehealth titration, subsidized meds, and community pharmacists who actually know what they’re dispensing. Until then, we’re just giving people a map to a destination they can’t reach. The drugs work. The system doesn’t.
Write a comment