Coronary Artery Disease Risk Calculator
This tool estimates your 10-year risk of developing coronary artery disease based on key medical factors. Use this information to discuss your heart health with your doctor.
Your Estimated Risk
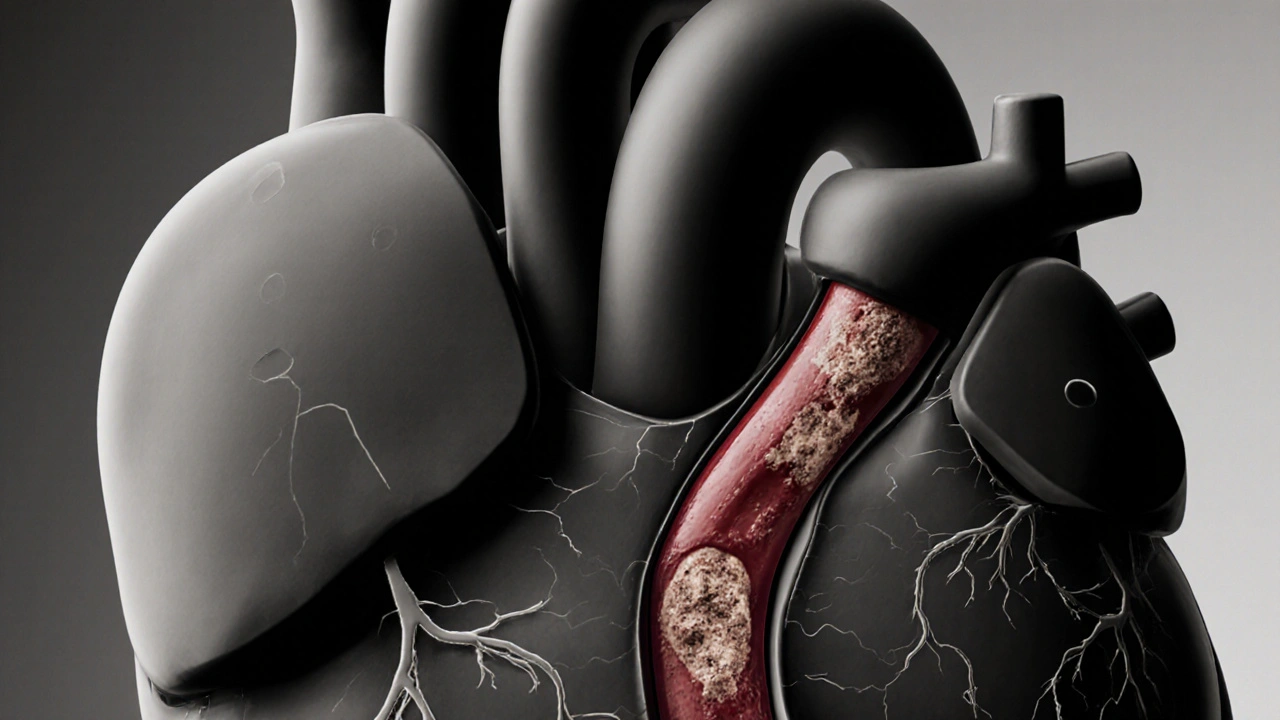
When the heart’s blood vessels get clogged, the whole body feels it. Coronary artery disease is a condition where plaque builds up inside the coronary arteries, narrowing them and reducing blood flow to the heart muscle. Understanding how it shows up, why it happens, and what you can do about it can make the difference between a painful flare‑up and a stable, healthier life.
What Exactly Is Coronary Artery Disease?
Atherosclerosis is the medical term for the plaque‑building process that underlies coronary artery disease. Over years, cholesterol, calcium, and cellular debris form sticky deposits on the inner walls of arteries. When these deposits grow, they stiffen the vessel and create a bottleneck for oxygen‑rich blood.
The heart relies on constant blood supply; even a small reduction can cause chest discomfort, while a sudden blockage can trigger a heart attack.
Typical Symptoms to Watch For
Symptoms vary from person to person, and some people never notice any until an event occurs. The most common signs include:
- Chest pressure or tightness (often described as “angina”) - Angina usually appears during physical activity or emotional stress and eases with rest.
- Shortness of breath, especially when climbing stairs or after a meal.
- Fatigue or dizziness that isn’t linked to other causes.
- Pain radiating to the left arm, jaw, neck, or back.
- Unexplained sweating or nausea during exertion.
Because symptoms can be vague, many patients only discover the disease after a more serious event like a myocardial infarction (heart attack).
Root Causes and Risk Factors
While genetics set the stage, lifestyle choices accelerate plaque buildup. Key contributors are:
- High LDL cholesterol - the “bad” cholesterol that sticks to artery walls.
- Smoking - nicotine damages the endothelium and speeds up atherosclerosis.
- High blood pressure - forces more stress on arterial walls.
- Diabetes - high blood sugar fuels inflammation.
- Family history of early heart disease.
- Sedentary habits, obesity, and diets high in saturated fats.
Addressing these factors early can slow or even reverse plaque progression.
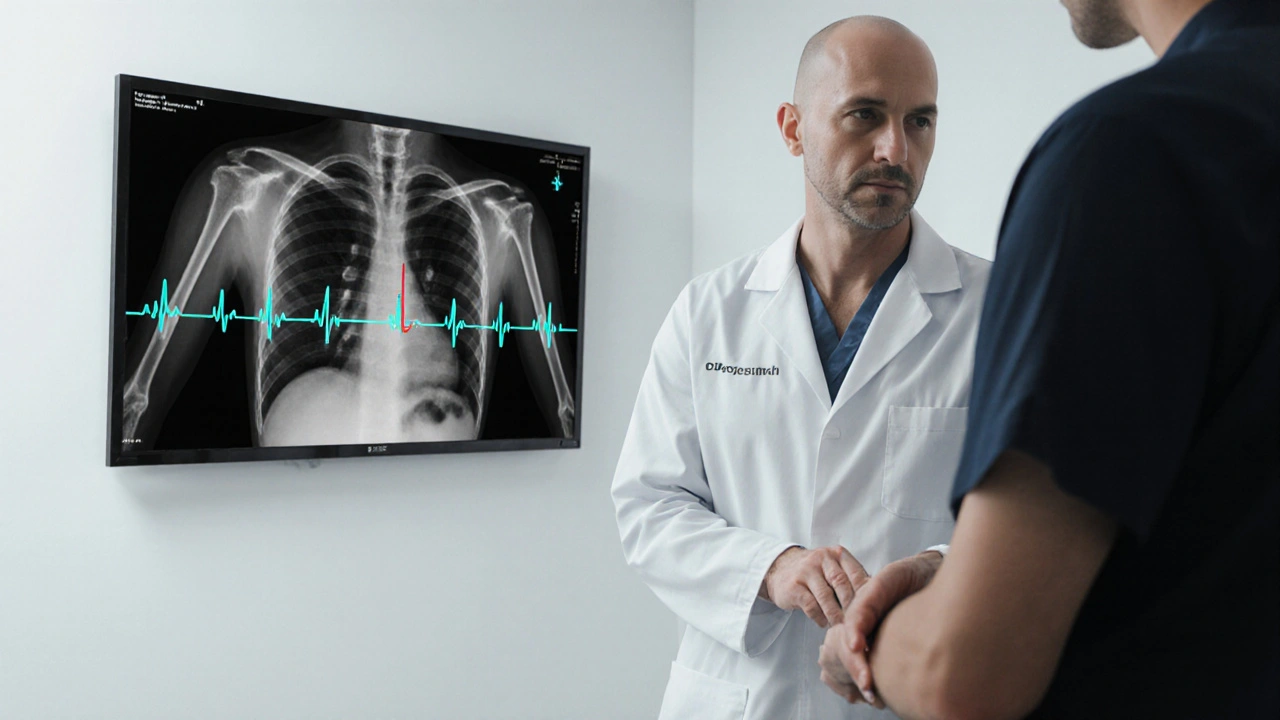
How Doctors Diagnose the Condition
Because symptoms can be subtle, doctors rely on several tests:
- Electrocardiogram (ECG) - records electrical activity and can spot abnormal heart rhythms or past heart attacks.
- Stress test - monitors heart function while you walk on a treadmill or pedal a bike.
- Coronary angiography - a dye‑based X‑ray that visualizes blockages directly.
- CT coronary calcium scan - measures calcium deposits as a proxy for plaque.
The results guide the treatment plan, balancing medication, lifestyle, and possible procedures.
Treatment Options Overview
Managing coronary artery disease usually involves a mix of medicines, minimally invasive procedures, and major surgery when needed. Below is a quick snapshot of what’s available.
| Treatment | How It Works | Typical Candidates | Recovery Time |
|---|---|---|---|
| Medications (Statins, Beta‑blockers) | Lowers cholesterol, reduces heart workload | Early‑stage disease, patients with mild blockages | None - daily pill |
| Percutaneous Coronary Intervention (PCI) | Balloon expands artery, stent keeps it open | Significant narrowing causing angina | 1‑2 days hospital stay |
| Coronary Artery Bypass Grafting (CABG) | Graft from another vessel bypasses the blockage | Multi‑vessel disease, left main artery blockage | 5‑7 days hospital, several weeks recovery |
Let’s dig deeper into each option.
Medication Management
First‑line therapy usually includes two drug families:
- Statins - lower LDL cholesterol by up to 50% and stabilize plaque.
- Beta‑blockers - reduce heart rate and blood pressure, decreasing oxygen demand.
- Other agents like ACE inhibitors, antiplatelet aspirin, and newer PCSK9 inhibitors may be added based on risk profile.
Patients often notice fewer angina episodes within weeks, and regular blood tests confirm cholesterol improvement.
Minimally Invasive Procedure: PCI
When medication isn’t enough, doctors may suggest Percutaneous Coronary Intervention. A thin catheter threads through a wrist or groin artery to the blockage. A tiny balloon inflates to compress plaque, and a stent-a metal mesh-holds the artery open.
Benefits include quick relief of chest pain and a short hospital stay. Risks are low but include bleeding at the access site, artery re‑narrowing (restenosis), or rare heart rhythm problems.
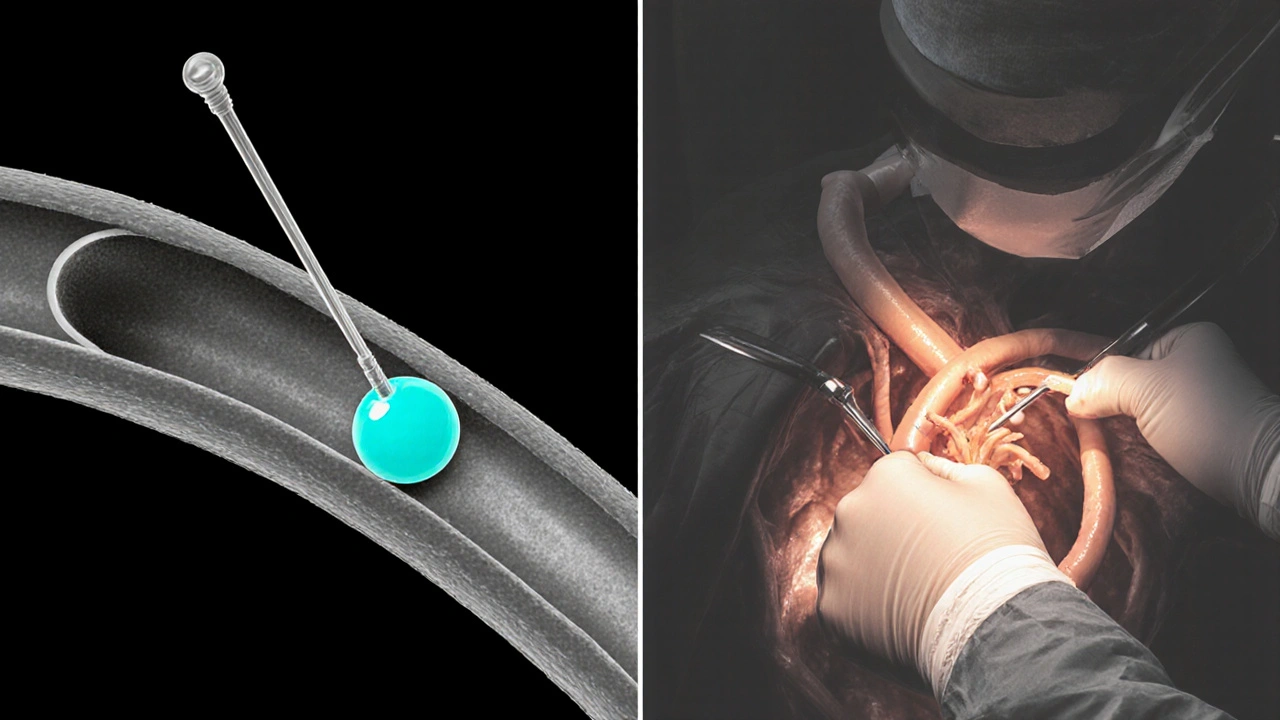
Open‑Heart Surgery: CABG
For extensive disease, especially when multiple arteries are narrowed, Coronary Artery Bypass Grafting may be the best choice. Surgeons take a healthy vessel from the leg or chest and graft it around the blocked segment, creating a new route for blood.
Although recovery takes longer, CABG offers durable relief and lower repeat‑procedure rates for high‑risk patients.
Lifestyle Changes That Make a Real Difference
Medicine and procedures work best when paired with daily habits that cut risk:
- Eat a heart‑healthy diet: plenty of fruits, vegetables, whole grains, lean protein, and omega‑3 fatty acids; limit saturated fats and processed sugars.
- Exercise regularly - aim for at least 150 minutes of moderate aerobic activity per week.
- Quit smoking - resources like nicotine patches or counseling increase success rates.
- Maintain a healthy weight - a BMI under 25 lowers pressure on the heart.
- Manage stress - mindfulness, yoga, or short daily walks can lower blood pressure.
These adjustments can lower LDL cholesterol by 10‑15% and improve blood pressure without medication.
Key Takeaways
- Coronary artery disease stems from atherosclerotic plaque that narrows heart arteries.
- Typical signs include chest pressure (angina), shortness of breath, and radiating pain.
- Major risk factors are high LDL, smoking, hypertension, diabetes, family history, and sedentary lifestyle.
- Diagnosis relies on ECG, stress testing, and imaging such as angiography.
- Treatment ranges from statins and beta‑blockers to PCI and CABG, complemented by diet, exercise, and smoking cessation.
Frequently Asked Questions
Can coronary artery disease be reversed?
While existing plaque can’t be fully removed, aggressive cholesterol‑lowering therapy (especially high‑intensity statins) and lifestyle changes can shrink plaque volume and stabilize it, reducing the chance of a heart attack.
What’s the difference between angina and a heart attack?
Angina is temporary chest pain caused by reduced blood flow; it usually fades with rest. A heart attack occurs when a plaque ruptures and completely blocks blood flow, causing permanent damage to heart muscle.
How often should I get my cholesterol checked?
Adults over 20 should have a lipid panel at least once every five years. If you have risk factors like family history or diabetes, your doctor may recommend yearly testing.
Is surgery always needed for severe blockages?
Not always. Many severe blockages can be opened with PCI and a stent. CABG is reserved for multi‑vessel disease, left main artery blockages, or when PCI results are unlikely to be durable.
Can I exercise if I have coronary artery disease?
Yes, regular aerobic activity is a cornerstone of treatment. Start slowly, follow your doctor’s guidance, and consider a cardiac rehab program to ensure safe progression.

16 Comments
Oh dear, the world drifts further into apathy while arteries clog like ignored traffic jams-our very hearts become silent testimonies to a society that refuses responsibility 😤.
Coronary artery disease (CAD) represents a progressive atherosclerotic process wherein lipid-laden plaques accrete within the intimal layer of the epicardial vessels, thereby compromising myocardial perfusion. The pathophysiology initiates with endothelial dysfunction, often precipitated by oxidative stress and shear‑force abnormalities. Subsequently, low‑density lipoprotein (LDL) particles infiltrate the subendothelial space, become oxidized, and trigger an inflammatory cascade involving macrophages and T‑lymphocytes. Foam cell formation ensues, contributing to the lipid core of the developing atheroma. Over time, smooth‑muscle cell migration and extracellular matrix deposition thicken the fibrous cap, which may remain stable or become vulnerable to rupture. Plaque rupture exposes thrombogenic material, prompting platelet aggregation and thrombus formation that can acutely occlude the coronary lumen. Clinically, this cascade manifests as angina pectoris when myocardial oxygen demand outstrips supply, especially during exertion or emotional stress. In advanced stages, intermittent ischemia may evolve into myocardial infarction if the occlusion persists. Risk stratification relies on quantifying traditional factors such as hyperlipidemia, hypertension, diabetes mellitus, tobacco use, and familial predisposition. Contemporary guidelines advocate aggressive lipid‑lowering therapy, most notably high‑intensity statins, to achieve target LDL levels below 70 mg/dL. Adjunctive agents-including PCSK9 inhibitors, ezetimibe, and omega‑3 fatty acids-offer additional plaque‑stabilizing benefits. Non‑pharmacologic interventions, such as the Mediterranean diet, regular aerobic exercise, and stress‑reduction techniques, synergistically attenuate disease progression. Diagnostic modalities encompass resting electrocardiography, stress‑induced imaging, coronary computed tomography angiography, and invasive coronary angiography when revascularization is contemplated. Revascularization options range from percutaneous coronary intervention with drug‑eluting stents to coronary artery bypass grafting for multivessel disease. Long‑term prognosis improves markedly when patients adhere to evidence‑based medical therapy and lifestyle modifications, underscoring the critical role of comprehensive secondary prevention.
The article accurately delineates the clinical spectrum of coronary artery disease and appropriately emphasizes a multimodal therapeutic approach.
Let me tell you, embracing a heart‑healthy lifestyle isn’t just wise-it’s an act of self‑empowerment that can dramatically shift outcomes, so grab those veggies, hit the treadmill, and watch that cholesterol tumble with relentless enthusiasm!
Honestly, the way most people treat their arteries is akin to setting fire to a priceless painting and then wondering why the smoke chokes them – a spectacularly reckless circus of bad habits and denial.
Friends, if we look at the broader picture, the integration of dietary adjustments, regular physical activity, and diligent medication adherence forms a triad that not only slows plaque accumulation but also fosters a community of support where each individual’s success story becomes a beacon for others navigating the same cardiovascular journey.
Wow!!! This guide is absolutely 🔥-it breaks down the scary stuff into bite‑size pieces, makes the science feel so real, and pumps you up to take charge of your heart health-let's do this!!!
Great summary! 😊
Scott, while your vivid metaphor certainly captures attention, it’s also vital to remember that education, rather than condemnation, tends to empower patients; by providing clear, evidence‑based guidance on diet, exercise, and medication adherence, we can transform fear into informed action and ultimately reduce the burden of coronary artery disease across diverse populations.
Sure, the article is “accurate,” but have you considered that the pharmaceutical industry might be shaping these guidelines to ensure perpetual drug sales, thereby keeping the populace permanently dependent on their pills?
Oh, absolutely, because shouting about “grab those veggies” magically turns cholesterol into a unicorn-let’s ignore the genetic predispositions and socioeconomic barriers that actually dictate heart health outcomes.
Josue, your comprehensive breakdown is impressive; could you elaborate on how emerging imaging techniques like fractional flow reserve CT might further refine our risk assessments?
Lauren, your point about empowerment resonates deeply-perhaps the real hierarchy we’re battling isn’t just cholesterol, but an unseen network of policy decisions that silently dictate who gets access to preventive care and who remains in the shadows.
Jenna, your enthusiasm is contagious, yet the underlying data still require careful interpretation to avoid overgeneralization.
Soumen, the communal approach you champion aligns beautifully with many traditional health practices worldwide, where collective encouragement and shared meals play a pivotal role in sustaining heart‑healthy habits.
Sydney, your dramatization borders on melodrama, but perhaps that theatrical flair is the only language some will heed when confronting the silent menace of arterial blockage.
Write a comment