Workplace Antihistamine Safety Checker
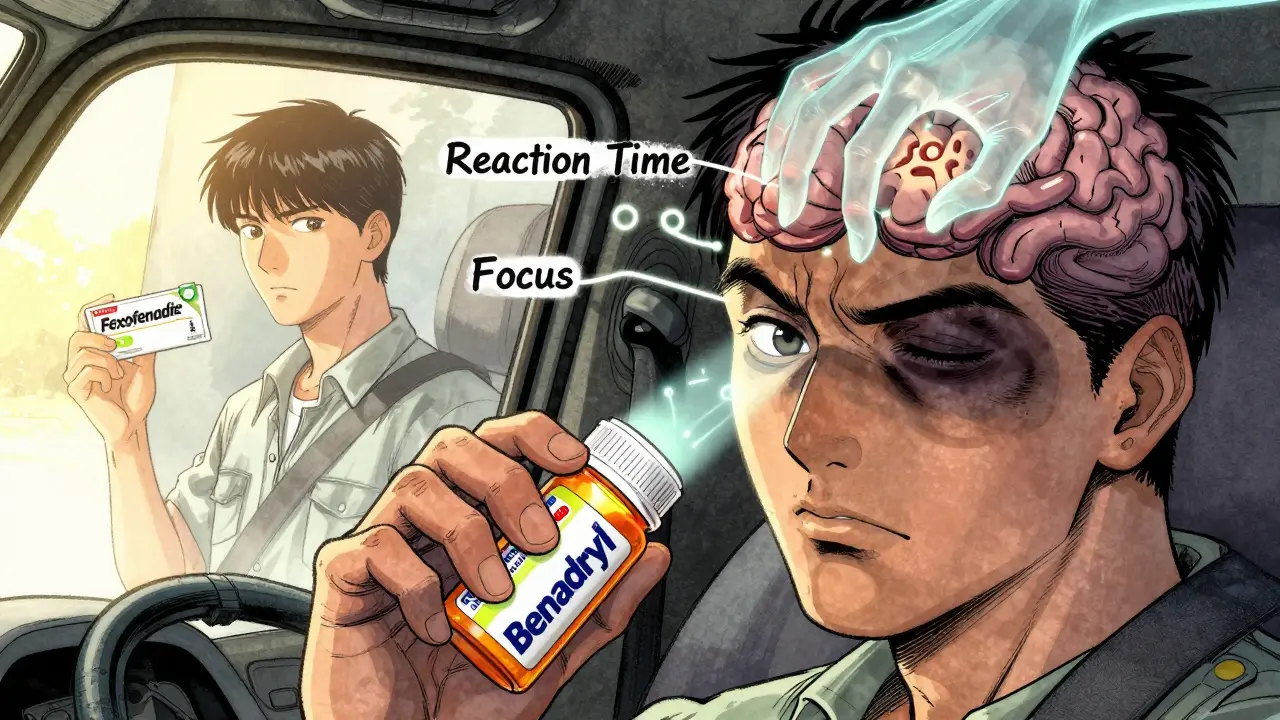
This tool helps you determine if your antihistamine is safe for work based on your job type and medication. Some antihistamines can impair your reaction time and focus, putting you and others at risk.
Results will appear here
Many people take antihistamines without thinking twice-especially during allergy season. But what if that pill you popped to stop your sneezing is also slowing down your reaction time, clouding your focus, and putting you-or others-at risk on the job? The truth is, not all antihistamines are created equal. Some are safe for daytime use. Others? They’re occupational hazards disguised as simple remedies.
Why Some Antihistamines Make You Dangerously Drowsy
First-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine (Chlor-Trimeton), and hydroxyzine (Atarax) were designed decades ago to block histamine, the chemical that triggers allergy symptoms. But here’s the catch: they also slip easily into your brain. That’s because they’re lipophilic-fat-soluble-and ignore the body’s natural barriers that keep foreign chemicals out of the central nervous system.
Inside your brain, histamine isn’t just about sneezes. It’s a key player in keeping you awake and alert. When these older antihistamines block brain histamine, they don’t just calm your nose-they quiet your mind. Studies show they can reduce reaction time by 25-30% and increase lane deviation in driving simulators by up to 50%. And here’s the scary part: you might not feel sleepy at all. A truck driver on Reddit reported failing a roadside cognitive test after taking Benadryl, saying, “I didn’t feel sleepy, but I couldn’t touch my nose with my finger.” That’s not paranoia-it’s science.
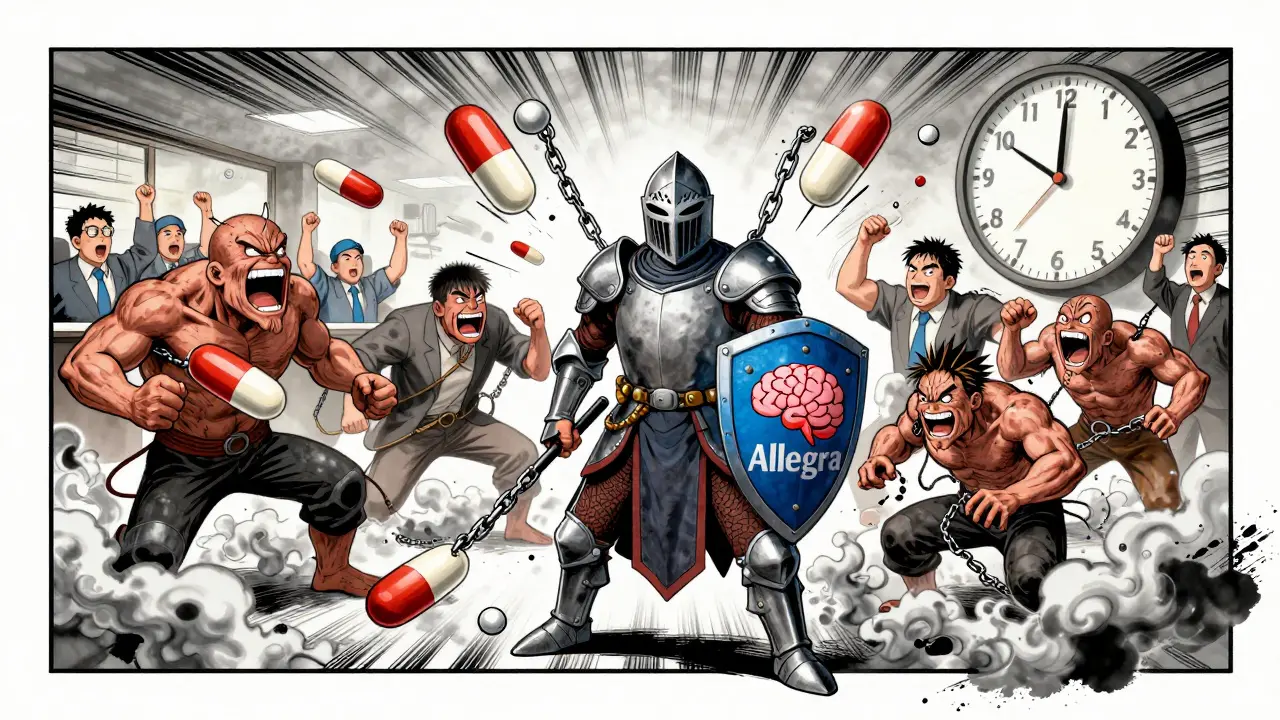
The Clear Difference: Second-Generation Antihistamines
Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) were engineered to fix this problem. They’re bulkier, less fat-soluble, and designed to be pumped out of the brain by P-glycoprotein transporters. In plain terms: they stay out of your central nervous system.
Research from 2013 in PubMed found that these newer drugs perform almost identically to placebo in psychomotor tests. Drivers on loratadine showed no measurable impairment. Pilots and truckers who switched from diphenhydramine to fexofenadine reported better focus, fewer near-misses, and no next-day grogginess. In fact, the FAA bans first-generation antihistamines for pilots. The Department of Transportation warns employers to treat them like alcohol-impairing performance even when users don’t feel it.
Who’s at Risk? It’s Not Just Drivers
Think you’re safe because you’re not behind the wheel? Think again. Construction workers operating heavy machinery, nurses administering medication, factory line operators, warehouse staff using forklifts, and even teachers managing classrooms-all face risks from sedating antihistamines.
One CDC study found that over a quarter of older adults fall each year. First-generation antihistamines are a major contributor. The dizziness, confusion, and slowed reflexes they cause increase fall risk by up to 40% in workers over 60. In manufacturing plants, a single delayed reaction can mean a hand caught in machinery or a misread gauge. A nurse on Nurse.com shared: “I switched from Benadryl to Claritin and noticed I was more alert during night shifts. I didn’t realize how much I’d been zoning out.”
The Hidden Danger: Delayed and Cumulative Effects
Many people think taking one pill at night won’t affect their next-day work. That’s a dangerous assumption. First-generation antihistamines have half-lives of 15 to 30 hours. That means if you take Benadryl at 8 p.m., half of it is still in your system at 11 a.m. the next day. Add a second dose later in the day? You’re stacking impairment.
And it gets worse with alcohol. Even one drink can double or triple the sedative effect. The FDA label on diphenhydramine explicitly warns against combining it with alcohol or other CNS depressants. Yet, surveys show 37% of users report next-day drowsiness, and 28% say they struggle to operate machinery even when they “feel fine.”
What Employers and Workers Need to Do
It’s not enough to rely on warning labels. The FDA requires them, but studies show they’re largely ignored. A 2022 FDA analysis found only 43% of first-generation antihistamine packaging includes clear timing advice, compared to 87% for second-generation options.
Here’s what works:
- Switch to non-sedating options. Loratadine, cetirizine, and fexofenadine are widely available over the counter and just as effective for allergies.
- Test new meds at home. Take a new antihistamine on a day off. Wait 6-8 hours. Try driving, typing fast, or balancing on one foot. If you feel off, don’t take it to work.
- Avoid first-generation antihistamines in safety-sensitive jobs. If your job involves operating machinery, driving, or handling hazardous materials, choose only second-generation options.
- Wait 24 hours after taking sedating antihistamines. The National Sleep Foundation recommends this for anyone returning to safety-sensitive duties. Don’t gamble with your focus.
Companies with safety-sensitive operations are catching on. As of 2023, 41% of Fortune 500 companies include antihistamine guidelines in their occupational health policies. Some require employees to disclose antihistamine use. Others offer free non-sedating alternatives through workplace clinics.
Real Numbers, Real Consequences
The U.S. National Highway Traffic Safety Administration estimates 100,000 police-reported crashes each year are caused by drowsiness. That’s likely an underestimate. Many drivers don’t admit to taking antihistamines after a crash, and toxicology screens aren’t always done.
Autopsy data from pilot crashes shows first-generation antihistamines are the most common medication found in their systems. Meanwhile, second-generation antihistamines appear in less than 2% of aviation accident reports. That’s not coincidence-it’s pharmacology.
Market trends reflect the shift. In 2022, second-generation antihistamines made up 68% of the global market. Sales of Benadryl are declining. Sales of Allegra and Claritin are rising. Why? Because people are learning the hard way that feeling fine doesn’t mean you’re safe.
What to Take Instead
Here’s a quick guide to safer choices:
| Medication | Generation | Brain Penetration | Half-Life | Impairment Risk | Workplace Safe? |
|---|---|---|---|---|---|
| Diphenhydramine (Benadryl) | First | High | 15-30 hours | High | No |
| Chlorpheniramine (Chlor-Trimeton) | First | High | 12-24 hours | High | No |
| Hydroxyzine (Atarax) | First | High | 14-20 hours | High | No |
| Loratadine (Claritin) | Second | Very Low | 8-12 hours | Minimal | Yes |
| Cetirizine (Zyrtec) | Second | Low | 8-10 hours | Low (some mild drowsiness in 10-15% of users) | Yes (with caution) |
| Fexofenadine (Allegra) | Second | Very Low | 11-15 hours | Minimal | Yes |
| Bilastine | Second (newer) | Very Low | 14 hours | Minimal | Yes |
For most people, loratadine or fexofenadine are the best choices. They work just as well for allergies, cost about the same, and won’t sabotage your focus.
Final Reality Check
You’re not being dramatic if you say you’re safer without Benadryl. You’re being smart. The science is clear: sedating antihistamines impair you more than most people realize-and often without warning. Your brain doesn’t feel sleepy, but your reaction time, judgment, and coordination are all slipping.
There’s no benefit to risking a crash, a fall, or a mistake on the job just to avoid a runny nose. The alternatives exist. They’re affordable. They’re effective. And they won’t put your life-or someone else’s-at risk.
If you take antihistamines regularly for allergies, asthma, or even sleep, ask yourself: Am I choosing safety-or just convenience?
Can I still take Benadryl if I take it at night?
Taking Benadryl at night doesn’t guarantee you’ll be safe the next day. Its half-life can be up to 30 hours, meaning significant amounts remain in your system the following morning. Even if you don’t feel sleepy, your reaction time and coordination may still be impaired. For safety-sensitive jobs, avoid it entirely-even if taken at night.
Is Zyrtec safe for work?
Cetirizine (Zyrtec) is a second-generation antihistamine and generally safe for most workplaces. However, about 10-15% of users still report mild drowsiness. If you’re in a high-risk job-like driving, operating machinery, or working at heights-test it at home first. If you feel even slightly sluggish, switch to fexofenadine or loratadine instead.
Do all antihistamines make you drowsy?
No. Only first-generation antihistamines-like diphenhydramine, chlorpheniramine, and hydroxyzine-cause significant drowsiness because they cross into the brain. Second-generation antihistamines like loratadine, fexofenadine, and bilastine are designed to stay out of the brain and rarely cause impairment.
Can I combine antihistamines with alcohol?
Never. Alcohol multiplies the sedative effects of first-generation antihistamines, increasing impairment beyond what either substance causes alone. Even one drink can turn a manageable dose into a dangerous one. The FDA warns against this combination for a reason.
What should I do if my doctor prescribes a sedating antihistamine?
Ask if a non-sedating alternative is available. Many doctors prescribe diphenhydramine out of habit, not because it’s the best choice. Mention your job duties and ask for a safer option. If your job involves driving, machinery, or safety-critical tasks, you have the right to request a medication that won’t impair you.
Are there laws against driving on antihistamines?
Yes. In the U.S., all 50 states have laws against driving under the influence of any drug that impairs your ability to operate a vehicle safely-including sedating antihistamines. If you’re in a crash and testing positive for diphenhydramine, you can be charged with DUI, even if you took it as directed.


10 Comments
Okay, but like… have you ever tried to function in a world where your sinuses are screaming and your eyes are bulging out of your skull? I get it, Benadryl’s a trap-but sometimes, you just need to breathe. I switched to Zyrtec, and honestly? I still feel like a zombie… just a slightly less dangerous one. I’m not saying we shouldn’t care about safety-I’m saying we shouldn’t pretend this is a clean choice.
It is an egregious oversight of corporate occupational health protocols that first-generation antihistamines remain OTC without mandatory cognitive impairment disclaimers on packaging. The pharmacokinetic profile of diphenhydramine is a neuropharmacological liability-its lipophilicity enables BBB penetration, and its antagonism of H1 receptors in the CNS induces psychomotor retardation indistinguishable from mild intoxication. Employers are legally liable for negligence when employees are permitted to operate machinery under its influence. This is not a suggestion-it is a regulatory imperative.
It’s funny, isn’t it? We’ve built entire systems-air traffic control, nuclear plants, surgical suites-on the assumption that humans are rational, alert, and consistent. And yet we hand out a pill that quietly, invisibly, dismantles all of that… and then act surprised when someone makes a mistake. We don’t blame the drug. We blame the person. But the drug was the silent saboteur. We’ve outsourced our attention to chemistry, and now we’re shocked when the chemistry fails us. What does that say about our relationship with control?
zyrtec is fine i guess but i just take allegra and im fine. also benadryl is for sleep bro. why are you even taking it during the day? like… what are you even doing?
To the person who said Zyrtec still makes them feel like a zombie: you’re not alone. And you’re not weak. About 1 in 7 people metabolize cetirizine differently-it hits them harder. That’s why I always tell my patients: don’t assume ‘second-gen’ means ‘zero effect.’ Test it. Sit in your driveway for 30 minutes after taking it. Can you tie your shoes without looking? Can you count backward from 100 by 7s? If not, don’t go to work. Your job doesn’t need your sacrifice-it needs your full presence. And you deserve to be safe while doing it.
Can we just admit that Americans treat medicine like candy? You wouldn’t drink before a shift. But you’ll pop a Benadryl like it’s a Skittle? Meanwhile, Canadians and Europeans have been requiring pharmacist counseling on sedating antihistamines for decades. We’re not just behind-we’re embarrassingly careless. The FAA bans these drugs for pilots. Why? Because they’re not stupid. We should be so lucky to have that level of common sense.
i work in a warehouse and i used to take benadryl every night because my allergies were killing me. last month i switched to claritin and honestly? i didn’t even notice the difference in my sneezing… but i noticed i stopped dropping boxes. i stopped zoning out during safety briefings. i even started noticing the little things-like when someone’s tool was out of place. i didn’t know i was that impaired. i’m not proud i waited this long to change. but i’m glad i did.
My dad’s a retired trucker. He told me he used to take Benadryl to stay awake on long hauls. I thought he was joking. Turns out, he wasn’t. He said he’d pull over just to stare at a tree for 20 minutes because his brain felt like it was underwater. He didn’t crash-but he came close. Now he takes Allegra. Says he feels like he’s got his brain back. I told him he should write a book. He said, ‘Nah. Just tell people to stop being dumb.’ I think he’s right.
There’s a quiet dignity in choosing safety over convenience. It’s not flashy. It doesn’t make headlines. But it’s the kind of choice that keeps people alive. I’ve worked in emergency response for 18 years. I’ve seen the aftermath of ‘just one pill.’ I’ve held the hands of people who didn’t realize they were impaired until it was too late. This isn’t about being perfect. It’s about being responsible. And if you’re reading this and you’ve ever taken diphenhydramine before a shift-you’re not a bad person. You’re just someone who didn’t know. Now you do.
What’s wild is that we’ve accepted this as normal. We don’t think twice about popping a pill that makes us slower than a drunk person. But we’ll shame someone for drinking one beer. Why? Because the pill is legal. Because it’s ‘natural.’ Because it’s in the medicine cabinet. But the danger? It’s identical. Maybe we need to stop calling it ‘allergy medicine’ and start calling it ‘performance-risk medication.’ Then maybe we’d take it seriously.
Write a comment