Skipping a pill because you’re running late, feeling fine, or just forgetting-it happens. But when it’s your prescription medication, even one missed dose can undo weeks of progress. It’s not about being perfect. It’s about keeping your body in the right zone-where the drug works, not where it fails.
Why Timing Matters More Than You Think
Your body doesn’t work on a schedule you pick. It works on chemistry. Every medication you take is designed to stay at a certain level in your bloodstream. Too little, and the drug can’t do its job. Too much, and you risk side effects or toxicity. Timing isn’t a suggestion-it’s a requirement built into the science of how your body absorbs, uses, and clears the drug.Take antibiotics. You feel better after three days? That’s great-but the bacteria aren’t gone. Stopping early lets the toughest ones survive. They multiply. Next time, they won’t respond to the same drug. That’s how antibiotic resistance starts. The CDC says you must finish every course, even if symptoms vanish. Skipping doses doesn’t save you time-it saves the bacteria.
Same goes for blood pressure pills. High blood pressure doesn’t give you warning signs. You don’t feel it. But it’s quietly damaging your heart, kidneys, and arteries. If you skip a dose, your pressure spikes. Do it often enough, and you increase your risk of stroke or heart attack. The American Heart Association says nearly half of U.S. adults have high blood pressure. Most of them are on meds. And most of those who die from preventable complications didn’t take their pills regularly.
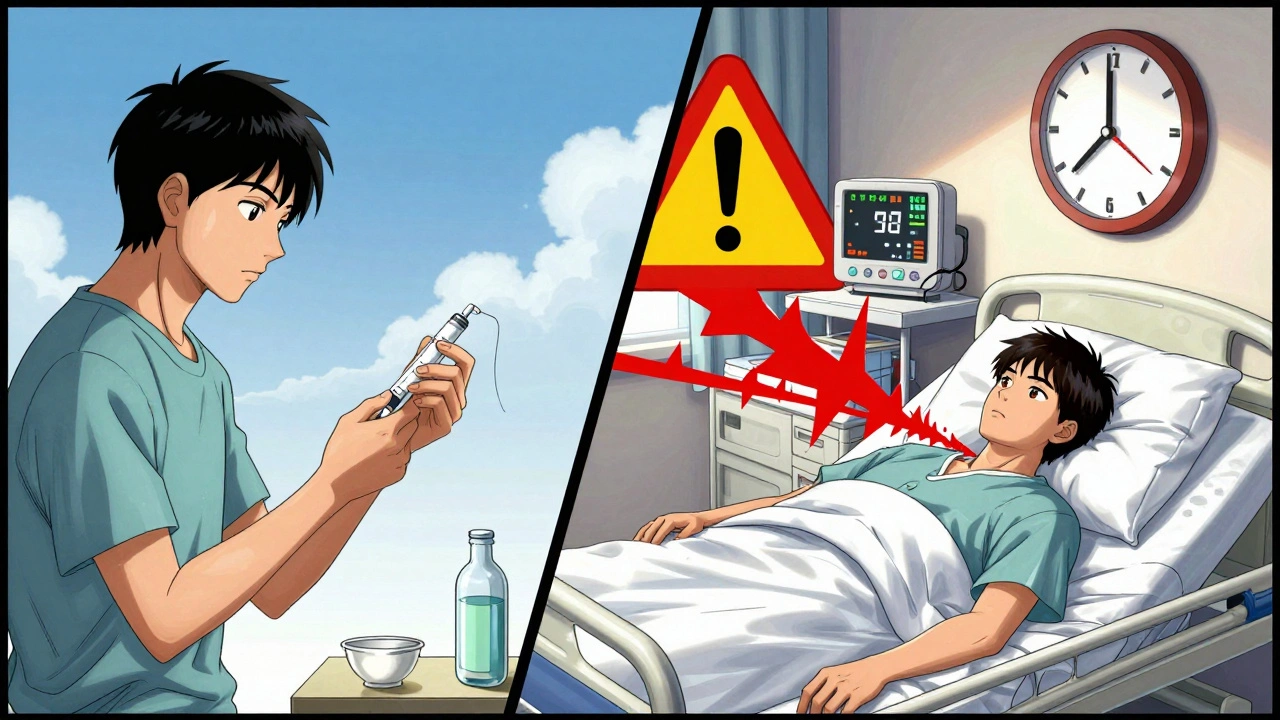
Medicines That Can’t Wait
Not all pills are created equal. Some need to be taken at exact times-or they become dangerous.- Warfarin (blood thinner): Your INR level must stay in a narrow range. Skip a dose? You could clot. Take two by accident? You could bleed out. Timing matters more than the dose itself.
- Insulin: Take it before a meal? Good. Take it after? Your blood sugar crashes. Take it on an empty stomach? You risk severe hypoglycemia. This isn’t optional-it’s life-or-death.
- Immunosuppressants (after transplant): One missed dose can trigger your body to attack the new organ. Rejection can happen fast. No second chances.
- Seizure meds: Even one skipped dose can trigger a seizure. For some, it’s like flipping a switch.
These aren’t edge cases. They’re common. If you’re on any of these, you’re not just managing a condition-you’re managing a tightrope walk. And timing is your safety line.
Why People Skip-And What Really Happens
People skip for reasons that make sense on the surface:- "I feel fine." But high blood pressure, diabetes, and cholesterol don’t announce themselves. Feeling good is a sign the medicine is working-not that you don’t need it.
- "I forgot." A 2022 study found that 40% of adults miss at least one dose per week. For those on five or more medications, adherence drops by 16% for every extra pill per day.
- "The side effects are bad." Some side effects fade after a week. Others can be managed. But stopping cold? That’s worse.
- "It’s too expensive." Skipping doses to stretch a prescription doesn’t save money. It leads to ER visits, hospital stays, and longer recovery times. One missed dose can cost $500 in emergency care.
Real consequences aren’t theoretical. Dignity Health reports patients who skipped heart meds ended up back in the hospital with heart failure. Others developed kidney damage from uncontrolled diabetes. A family doctor in Alabama found that the #1 reason patients messed up their meds? They didn’t understand the instructions. Not because they were careless. Because no one explained it clearly.
How to Get It Right-Without Stress
You don’t need to be a robot. You need a system.- Use a pill organizer. Weekly boxes with morning, afternoon, evening slots are free at most pharmacies. Fill them once a week. If the slot’s empty, you know you missed it.
- Set phone alarms. Name them: "Take BP pill," "Insulin before lunch." Don’t just say "Meds." Be specific.
- Link it to habits. Brush your teeth? Take your pill right after. Drink coffee? Take your pill with it. Your brain learns routines faster than schedules.
- Ask your pharmacist to simplify. If you’re on 8 pills a day, ask if any can be combined or switched to once-daily versions. Every reduction improves adherence.
- Use the "teach-back" method. After your doctor explains your meds, say: "So, to make sure I got it right-I take this pill every morning with food, and this one at night on an empty stomach. Is that correct?" If they nod, you’re golden.
Pharmacists are your secret weapon. They don’t just fill prescriptions-they check for timing conflicts, side effect risks, and duplicate meds. Ask for a Medication Therapy Management (MTM) session. It’s free if you’re on Medicare Part D.
The Bigger Picture: It’s Not Just About You
Skipping doses doesn’t just hurt you. It costs the system. The U.S. spends $300 billion a year on preventable hospitalizations-and medication non-adherence is a major driver. That’s not just money. It’s time lost, families stressed, emergency teams rushed, and lives cut short.Million Hearts, a national campaign launched in 2012, is trying to prevent one million heart attacks and strokes by 2027. One of their top strategies? Getting people to take their blood pressure and cholesterol meds exactly as prescribed. Why? Because it works. Consistent dosing cuts stroke risk by 40%. Heart attack risk by 30%.
This isn’t about discipline. It’s about design. Your body needs the right amount of medicine, at the right time, every single day. No exceptions.
What to Do If You Miss a Dose
Don’t panic. Don’t double up. Check the label. If it doesn’t say what to do, call your pharmacist. General rules:- If it’s close to your next dose (within 2-4 hours): Skip the missed one. Don’t double up.
- If it’s been longer than that: Take it as soon as you remember.
- For insulin, blood thinners, or seizure meds: Call your provider immediately. Never guess.
Keep a log. Note when you missed a dose and why. Over time, you’ll see patterns. Maybe you always forget after travel. Or after a night out. Plan for it.
What happens if I skip a dose of my blood pressure medicine?
Skipping a dose can cause your blood pressure to spike, even if you feel fine. These spikes put stress on your heart, kidneys, and blood vessels. Over time, this increases your risk of stroke, heart attack, or kidney damage. One missed dose won’t cause immediate harm-but repeated misses do. Consistency is what keeps your pressure stable.
Can I take my meds with food if the label says "on an empty stomach"?
No. Some medications are absorbed differently depending on whether your stomach is full or empty. For example, certain antibiotics like tetracycline bind to calcium in dairy, making them useless. Others, like some thyroid meds, won’t work if taken with coffee or fiber. Always follow the label. If you’re unsure, ask your pharmacist.
Why do I need to take antibiotics even after I feel better?
Antibiotics kill the weakest bacteria first. The strongest ones survive if you stop early. These survivors multiply and become resistant. That’s how superbugs form. You might feel better, but the infection isn’t gone. Finishing the full course stops resistance and prevents the infection from coming back stronger.
I’m on 6 different pills a day. How do I keep track?
Start with a pill organizer. Fill it once a week. Set phone alarms for each dose with clear names like "Diabetes AM" or "Blood thinner PM." Ask your pharmacist if any pills can be switched to once-daily versions. Many can. Also, request a Medication Therapy Management (MTM) session-your pharmacist will review all your meds for timing conflicts and simplify your routine.
Is it okay to skip doses if my meds are expensive?
No. Skipping doses to stretch your supply is dangerous and costly. A single hospitalization from uncontrolled high blood pressure or diabetes can cost thousands. Talk to your doctor or pharmacist about generic alternatives, patient assistance programs, or mail-order pharmacies. Many drugmakers offer free or low-cost meds for qualifying patients. Don’t risk your health to save money-there are safer options.
Final Thought: This Isn’t About Perfection
You’re not failing if you miss a dose. You’re human. But every time you skip, you’re gambling with your health. The goal isn’t to be flawless. It’s to build a routine so strong that missing a dose becomes the rare exception-not the norm.Set your alarms. Use your pillbox. Talk to your pharmacist. Ask questions. Your body doesn’t need you to be perfect. It just needs you to show up-on time, every day.


13 Comments
Oh wow, another ‘meds are sacred’ sermon. I’m sure the pharmaceutical lobby paid you in Bitcoin to write this. 🙄
Pharmacokinetic non-adherence is a primary driver of subtherapeutic plasma concentrations, leading to therapeutic failure and accelerated resistance dynamics. The pharmacodynamic window for most chronically administered agents is narrow-deviations ≥15% from scheduled dosing induce significant pharmacological drift. This isn’t anecdotal-it’s evidenced by population-level PK/PD modeling from FDA post-marketing surveillance data.
Antibiotic stewardship protocols are grounded in MIC/MBC thresholds, not subjective symptom resolution. Skipping doses selects for efflux pump upregulation and beta-lactamase expression. You’re not ‘saving time’-you’re engineering superbugs.
Warfarin’s narrow TI (therapeutic index) demands INR monitoring within ±0.5 of target. One missed dose can shift your coagulogram into the danger zone. PT/INR isn’t a suggestion-it’s a biological feedback loop you’re actively sabotaging.
Insulin pharmacodynamics are circadian-phase-dependent. Delayed dosing alters hepatic glucose output kinetics. Hypoglycemia isn’t a ‘side effect’-it’s a metabolic cascade triggered by temporal mismatch.
Immunosuppressants like tacrolimus have zero tolerance for variability. Trough levels must be maintained within 5–10 ng/mL. A single missed dose can initiate alloreactive T-cell activation. Rejection isn’t ‘possible’-it’s statistically inevitable with inconsistent dosing.
Seizure meds? GABA modulation is time-sensitive. Even 4-hour delays can lower seizure threshold. The brain doesn’t care if you were ‘busy’-it only responds to neurochemical gradients.
Non-adherence costs $500B annually in the US alone. That’s not ‘expensive meds’-that’s preventable ICU admissions, stroke rehab, and transplant rejections. You’re not saving money-you’re funding hospital CFO bonuses.
Using a pill organizer? Basic. Setting alarms? Elementary. MTM sessions? Free under Medicare Part D. If you can’t manage this, maybe you shouldn’t be managing your own life.
You got this. Even one consistent day makes a difference. 💪
I used to skip my blood pressure meds all the time because I ‘felt fine.’ Then I had a scare. Now I set five alarms and keep my pills next to my toothbrush. It’s not perfect, but it’s better. You’re not alone. 🤍
Bro. I used to be the guy who skipped his meds ‘because I felt good.’ Then I ended up in the ER with a BP of 210/120. My doctor looked at me like I’d just tried to microwave my cat. 😅
Now I use a pillbox, set alarms named ‘DONT-DIE-AM’ and ‘DONT-DIE-PM,’ and my pharmacist knows my face. It’s not sexy. But it’s how you stay alive.
Also-pharmacists are wizards. Ask them for MTM. Free. No BS. They’ll cut your 8 pills down to 3. I swear.
You’re not lazy. You’re just not taught right. And that’s on the system. Not you.
im not sayin u r wrong but like… my grandpa skipped his warfarin for 3 days ‘cause he forgot and then he was fine? idk man. maybe its just me?
Wait-so if I take my insulin 20 mins late, does that count as ‘skipping’? Or is it more like… ‘delayed administration’? Asking for a friend who’s trying to be scientifically precise and not feel guilty. 😅
This entire post is a beautifully articulated, clinically sound, and ethically imperative exposition on the bioethical imperative of pharmaceutical adherence. It reveals the terrifying fragility of modern pharmacotherapy when subjected to the capriciousness of human forgetfulness, economic precarity, and systemic healthcare neglect. The fact that we reduce life-sustaining regimens to ‘set an alarm’ is a societal indictment. We have outsourced our biological autonomy to a pill, and yet we treat it with the reverence of a forgotten grocery list. This isn’t about discipline-it’s about dignity. And dignity, in the face of chronic illness, is not optional. It is the last vestige of selfhood we retain. If you skip a dose, you are not just risking your health-you are surrendering your personhood to the algorithm of neglect.
Wow. So now we’re all supposed to be pharmaceutical robots? Next you’ll tell me to wear a sensor that pings my doctor every time I blink wrong.
Let me guess-you also think people who take their meds regularly are ‘good’ and those who don’t are ‘bad.’ That’s not medicine. That’s moralizing with a stethoscope.
What about the guy who can’t afford his insulin? What about the single mom who forgets because she’s working two jobs and her kid threw up at 3am?
Stop shaming. Fix the system.
i think u r right but also… life is messy. i take my bp med but sometimes i forget after i eat biryani and fall asleep. then i wake up at 2am and take it. is that bad? i dont know. maybe my body is smarter than the label. 🤔
Medication timing is science. Skipping is gamble. Simple.
why are u making this so dramatic. i skip meds all the time. i still alive. ur post is just fearmongering with a pharmacy logo.
I cried reading this. Not because I’m perfect-I’m not. I missed my seizure meds last month because my cat knocked over my pillbox and I was too exhausted to clean it up. I had a seizure. In public. At Target.
I didn’t die. But I felt like I lost myself.
Now I keep a backup pillbox in my purse. I set alarms with my mom’s voice saying ‘PLEASE TAKE YOUR PILLS, BABY.’
It’s not about being perfect. It’s about showing up for the version of you that wants to see tomorrow.
And if you can’t? That’s okay. Just call someone. Or your pharmacist. Or me. I’ll send you a meme. 🫂
Write a comment