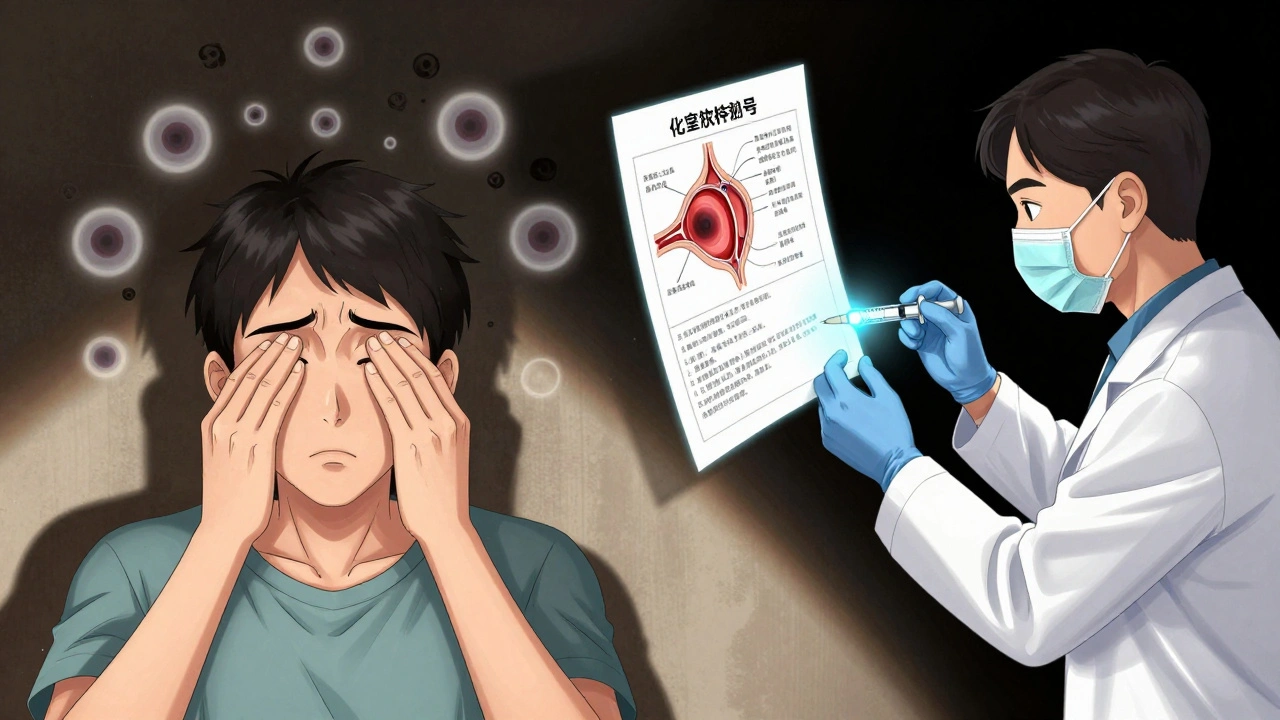
Uveitis is not just a red eye. It’s inflammation deep inside the eye - in the uvea, the middle layer that feeds the retina and iris. Left untreated, it can lead to permanent vision loss. And it happens faster than most people realize. One day, your vision feels blurry. The next, light hurts your eyes. You see floaters like spiderwebs. By the time you think to see a doctor, damage may already be done. This isn’t rare. Uveitis is the third leading cause of blindness worldwide. Yet many people don’t know what it is - or how urgent it is.
What Exactly Is the Uvea?
The uvea isn’t one part. It’s three: the iris (the colored ring around your pupil), the ciliary body (which helps focus your lens), and the choroid (a layer packed with blood vessels that feeds the retina). Think of it like the wiring and fuel line of your eye. When inflammation hits here, it doesn’t just cause redness. It swells tissues, blocks fluid flow, and can scar the retina or optic nerve. That’s how vision fades - slowly, silently, and often without pain in the early stages.Four Types of Uveitis - And Why It Matters
Uveitis isn’t one condition. It’s grouped by where the inflammation lives:- Anterior uveitis (iritis): Affects the front - iris and ciliary body. This is the most common type, making up 75-90% of cases. Symptoms hit hard: red eye, sharp pain, light sensitivity, blurred vision. Often comes on suddenly. If treated fast, vision usually recovers.
- Intermediate uveitis (pars planitis): Hits the vitreous, the jelly-like fluid behind the lens. Floaters are the main sign. Pain is mild or absent. This form often becomes chronic, lasting months or years, and can cause macular edema - swelling in the center of your retina that blurs your central vision.
- Posterior uveitis: Inflammation in the choroid and retina. This is the most dangerous. It often affects both eyes, develops slowly, and can destroy retinal cells. Many people don’t notice symptoms until vision is already damaged. It’s frequently found during routine eye exams.
- Panuveitis: Inflammation in all layers at once. Symptoms combine everything - pain, floaters, blurred vision, light sensitivity. This is the most severe and hardest to treat.
Knowing which type you have changes everything - from treatment to prognosis. Anterior uveitis might clear in weeks. Posterior uveitis can take months of aggressive therapy.
What Causes Uveitis?
In about one-third of cases, doctors can’t find a cause. That’s called idiopathic uveitis. But when they can, here’s what they find:- Autoimmune diseases: Ankylosing spondylitis, lupus, multiple sclerosis, rheumatoid arthritis. Your immune system attacks your own eye tissue.
- Infections: Herpes simplex, shingles (herpes zoster), cytomegalovirus (CMV), syphilis, toxoplasmosis, histoplasmosis. These can wake up from dormancy and trigger inflammation.
- Trauma or surgery: A blow to the eye, a scratch, or even eye surgery can cause inflammation as a reaction to injury.
Here’s the catch: You might have an autoimmune disease and not know it. Uveitis can be the first sign of something deeper. That’s why doctors don’t just treat the eye - they look for clues elsewhere in your body.
Steroid Therapy: The First Line of Defense
Steroids are the backbone of uveitis treatment. They don’t cure the cause, but they stop the inflammation before it destroys your vision. How they’re given depends on where the inflammation is.- Topical eye drops (like prednisolone acetate 1%): Used for anterior uveitis. You might start with drops every hour, then taper over weeks. This works because the front of the eye is easy to reach.
- Periocular injections: Shots around the eye for intermediate uveitis. These deliver steroids directly to the vitreous, bypassing the need for systemic treatment.
- Oral steroids (like prednisone): For posterior uveitis or panuveitis. These work throughout the body, reaching the back of the eye. But they come with risks - weight gain, mood swings, high blood sugar, bone thinning.
- Intravitreal implants: Tiny devices placed inside the eye that slowly release steroids over months. Used for chronic cases where long-term treatment is needed without daily pills.
Doctors don’t just give steroids and walk away. They watch closely. Too little? Inflammation comes back. Too much? You risk cataracts or steroid-induced glaucoma - both of which can steal your vision, too. About 30-40% of long-term steroid users develop one or both.
When Steroids Aren’t Enough
If uveitis keeps coming back, or you can’t tolerate steroids, doctors turn to steroid-sparing therapies. These are drugs that calm the immune system without the side effects of steroids:- Methotrexate: Often used for chronic uveitis linked to autoimmune disease.
- Azathioprine: Helps reduce flare-ups over time.
- Biologics (like adalimumab): Target specific parts of the immune system. Used for severe, treatment-resistant cases.
These aren’t quick fixes. They take weeks to months to work. But they’re essential for people who need long-term control. Many patients go from monthly flare-ups to staying stable for years.
Warning Signs You Can’t Ignore
Don’t wait to see if it gets better. Uveitis doesn’t always hurt. But here’s when to act:- Red eye that doesn’t go away with rest or eye drops
- Floaters that suddenly multiply
- Blurred vision that comes on fast
- Pain that worsens when reading or focusing
- Sensitivity to light - even normal daylight feels too bright
If you have one or more of these, see an eye doctor within 24 hours. If you can’t get in, go to urgent care or the ER. Delaying treatment by even a few days can mean the difference between saving your vision and losing it.

What Happens If You Don’t Treat It?
Untreated uveitis doesn’t just cause blurry vision. It causes permanent damage:- Macular edema: Swelling in the central retina - the part you use to read, drive, recognize faces.
- Synechiae: The iris sticks to the lens or retina, distorting the pupil and blocking fluid drainage.
- Glaucoma: Pressure builds up inside the eye, crushing the optic nerve.
- Cataracts: Clouding of the lens - often caused by steroids, but also by chronic inflammation.
- Retinal detachment: The retina pulls away from the back of the eye.
These aren’t rare complications. They’re the norm if uveitis is ignored. The Lions Eye Institute calls it a "potentially sight-threatening problem" - and they’re right. Up to 15% of people with uveitis end up with significant vision loss.
Can You Prevent It?
You can’t prevent most cases - especially if they’re tied to autoimmune disease or infection. But you can prevent the damage:- Know your body. If you have an autoimmune condition, get regular eye checkups.
- Don’t ignore eye symptoms. Even mild blurriness or floaters after an injury or illness need checking.
- Protect your eyes. Wear safety glasses during sports or work that risks trauma.
- Treat infections early. Shingles, herpes, and syphilis can trigger uveitis if left unchecked.
There’s no magic pill. But catching uveitis early - and treating it aggressively - gives you the best shot at keeping your sight.
Is uveitis contagious?
No, uveitis itself is not contagious. You can’t catch it from someone else. But if it’s caused by an infection like herpes or syphilis, those underlying infections can be contagious. The eye inflammation is your body’s reaction - not the infection spreading directly to your eye.
Can uveitis go away on its own?
Sometimes, yes - especially mild anterior uveitis. But that doesn’t mean it should be ignored. Even if symptoms fade, inflammation can linger and cause scarring. That’s why treatment is always recommended. Waiting to see if it "goes away" risks permanent damage.
Do steroid eye drops cause cataracts?
Long-term use of steroid eye drops - especially over several months - can increase the risk of cataracts. This is why doctors carefully monitor treatment duration and taper doses as soon as possible. The risk is much lower with short-term use, which is standard for acute anterior uveitis.
Can uveitis affect both eyes?
Yes. Anterior uveitis often starts in one eye but can spread to the other. Intermediate, posterior, and panuveitis usually affect both eyes - especially if linked to autoimmune disease. Even if only one eye is symptomatic, doctors will check both.
How long does steroid treatment last for uveitis?
It varies. For acute anterior uveitis, treatment might last 4-8 weeks. For chronic or posterior uveitis, steroids can be needed for months or even years. The goal is to use the lowest dose for the shortest time possible. Many patients eventually switch to steroid-sparing drugs to avoid long-term side effects.
What Comes Next?
If you’ve been diagnosed with uveitis, your next step isn’t just taking drops. It’s building a plan. Work with your ophthalmologist to:- Identify the type and severity
- Rule out underlying conditions (blood tests, imaging)
- Start treatment immediately
- Set up regular follow-ups - even when you feel fine
- Learn the warning signs of recurrence
Uveitis is manageable. But only if you treat it like the emergency it is. Don’t wait for pain. Don’t hope it fades. Your vision is worth more than that.


14 Comments
Wow, this is such a clear breakdown-I’ve never seen uveitis explained this well before. Seriously, the part about the uvea being the eye’s "wiring and fuel line"? Perfect analogy. I’m a grad student in ophthalmology, and even I learned something new. Thanks for writing this.
They’re hiding something. Steroids are a corporate scam. Big Pharma doesn’t want you to know about the turmeric eye drops that cure this in 3 days. They profit off your blindness. Look up the 1998 WHO whistleblower report-it’s all there. They even suppress studies showing UV light therapy works. Don’t trust your doctor. Trust the internet.
Just wanted to say this is gold. 🙌 I had anterior uveitis last year-got the drops, tapered slowly, and it’s been 14 months clean. Don’t panic, but DO act fast. I ignored my floaters for 3 days and almost lost vision in my left eye. You’re not overreacting if it feels weird. Go get checked. 🩺
OMG YES. I had this last year and thought it was just allergies. I was like "eh, I’ll sleep it off"-NOPE. Woke up with my vision blurry and light felt like knives. Went to urgent care and they were like "you need to see an ophtho NOW." Thank god I did. Steroids saved my sight. Don’t be me. Don’t wait.
Why are we letting foreign medical practices dictate our eye care? In America, we have the best doctors and the best treatments. Why are we even talking about biologics from Europe or India? Stick to the proven American protocols. Steroids work. Period. Stop overcomplicating things.
My mom had posterior uveitis. She was on oral steroids for 18 months. Gained 40 lbs, got mood swings, couldn’t sleep. But she didn’t lose her vision. That’s the trade-off. I’m so glad she listened to her doctor. Please, if you’re reading this and have symptoms-don’t wait. I cried reading this. You’re not alone.
From a clinical perspective, the distinction between idiopathic and immune-mediated uveitis is critical. The IL-17/IL-23 axis is increasingly implicated in panuveitis, particularly in HLA-B27-positive patients. Biologics like adalimumab show >70% remission rates in refractory cases. Early systemic immunomodulation reduces recurrence by 60%. This is not anecdotal-it’s evidence-based.
Just go to the eye doctor. Seriously. Don’t wait. I’m not even joking.
It is rather unfortunate that the author has chosen to employ such a colloquial tone when discussing a condition of such grave clinical significance. The use of phrases like "spiderwebs" and "fuel line" is aesthetically pleasing, perhaps, but lacks the requisite scientific gravitas. One would hope for peer-reviewed terminology, not internet blog prose.
...but what if the inflammation is just your soul rejecting the modern world? I mean, think about it-your eyes are the windows to your spirit, right? And if you’re constantly staring at screens, absorbing trauma, living in a capitalist hellscape... isn’t the uveitis just your body screaming? Steroids are just a band-aid on a systemic collapse. We need to heal the planet, not just the retina...
Thank you for this. In India, many people ignore eye symptoms because they think it’s just tiredness. I showed this to my cousin-he went to the doctor yesterday after reading it. He had intermediate uveitis. Early treatment. Good outcome. Small things matter.
I’ve been managing chronic uveitis for six years now. Started with drops, moved to injections, then oral steroids, then methotrexate. I’m on adalimumab now. It’s not perfect-I still get flares, especially during stress or cold weather. But I haven’t lost vision. I used to think I’d be blind by 30. I’m 37. I drive. I read. I see my daughter’s face. This post? It’s not just information. It’s hope. Thank you for writing it. I’m sharing this with every support group I’m in.
weird how they say uveitis isnt contagious but then say herpes can cause it… so… if i get herpes from someone… and then get uveitis… is it kinda contagious? like… the uveitis is the result… but the thing that caused it… was contagious… so… is it contagious? i’m confused. maybe we need better words.
Why do people even care about this? Everyone’s just gonna go blind eventually anyway. Might as well enjoy the last few years of sight. Who needs to read or drive anyway? Just chill. It’s not that big a deal.
Write a comment