Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis aren’t just rare skin conditions-they’re life-threatening emergencies triggered by your own body’s reaction to medication. Think of them as extreme, unpredictable allergic responses that turn your skin and mucous membranes into raw, painful wounds. If you’ve ever taken an antibiotic, seizure medicine, or even a common painkiller like ibuprofen, you should understand what these conditions are, how they start, and why timing matters more than anything else.
It’s Not One Condition-It’s a Spectrum
Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) used to be thought of as two separate diseases. Now doctors know they’re part of the same deadly continuum. The only real difference? How much of your skin comes off.
SJS affects less than 10% of your body surface area. TEN? That’s more than 30%. There’s even a middle zone-10% to 30%-called SJS/TEN overlap. It sounds like a number game, but it’s not. Every extra percent of skin loss means higher risk of infection, organ failure, and death. TEN has a mortality rate near 25%. SJS? Around 10%. Those numbers aren’t just statistics-they’re real people in burn units, fighting for their lives.
The skin doesn’t just peel like a sunburn. It detaches in sheets. Blisters form, then burst. What’s left behind is raw, wet, oozing tissue-exactly like a severe burn. And it doesn’t stop at the skin. Your mouth, eyes, genitals, and throat are just as badly damaged. You can’t swallow. You can’t blink. You can’t breathe without pain.
How It Starts: The Silent Warning Signs
Most people don’t realize they’re heading toward disaster until it’s too late. The first signs look like the flu: fever, sore throat, burning eyes, cough, fatigue. You might think you’re coming down with a cold. But within 1 to 3 days, those symptoms shift. Red or purple spots appear on your chest and back. They spread fast. Then the blisters form.
One telltale sign? The Nikolsky sign. If you gently rub the skin near a lesion and it peels away, that’s a red flag. This doesn’t happen with regular rashes. It’s a hallmark of SJS/TEN. And if you have mouth sores that won’t heal, or your eyes feel like they’re full of sand, don’t wait. These are not minor side effects. They’re warning signals.
Medications are the main trigger-in over 80% of cases. The usual suspects? Carbamazepine (for seizures), allopurinol (for gout), sulfonamide antibiotics (like Bactrim), lamotrigine (for epilepsy and bipolar disorder), and NSAIDs like ibuprofen or naproxen. Even a single dose can set it off. And it doesn’t matter if you’ve taken the drug before. This reaction can happen on day one or after months of use.
Why Some People Are at Much Higher Risk
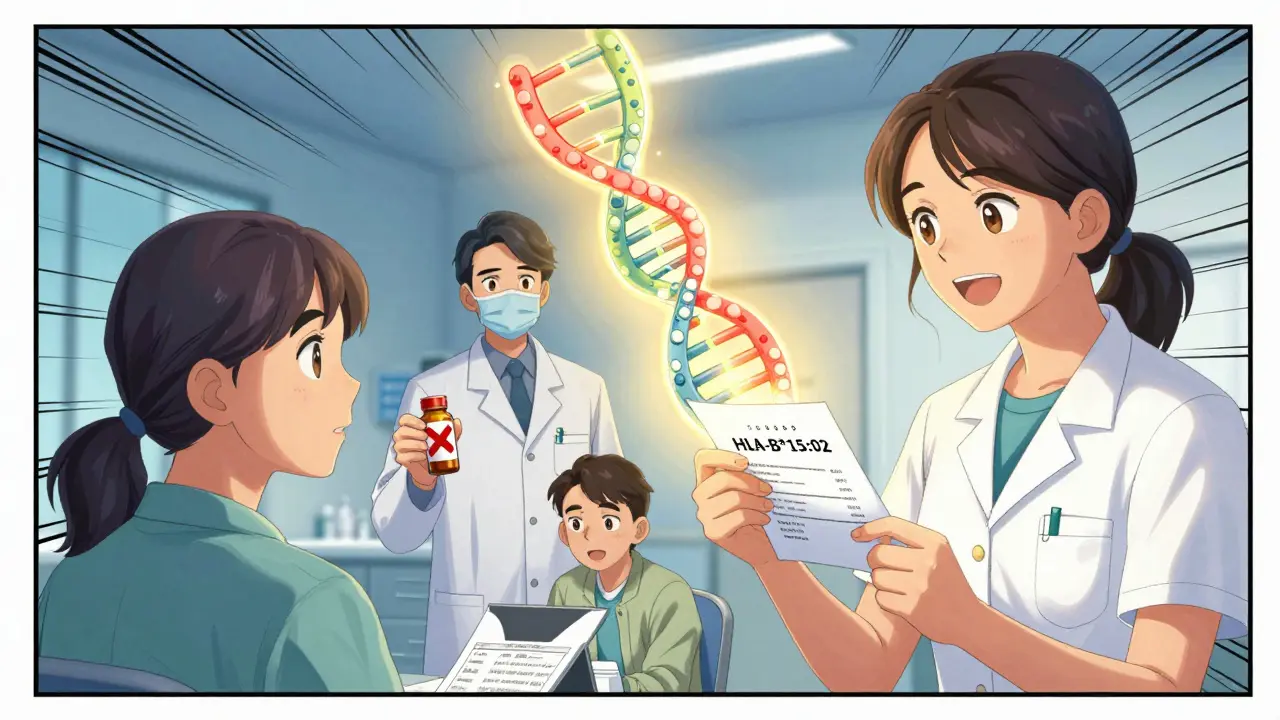
Not everyone who takes these drugs gets SJS/TEN. But some people are genetically wired to react badly. The biggest clue? Your genes.
If you’re of Asian descent and carry the HLA-B*15:02 gene, taking carbamazepine increases your risk by up to 1,000 times. That’s not a small chance-it’s a ticking time bomb. The same goes for HLA-B*58:01 and allopurinol. People with this gene variant are 80 to 580 times more likely to develop TEN.
Because of this, countries like Taiwan now require doctors to test for HLA-B*15:02 before prescribing carbamazepine. Since 2007, SJS/TEN cases from this drug dropped by 80%. In the U.S., the FDA now recommends screening for high-risk populations. If you’re prescribed one of these drugs and haven’t been tested, ask why. This isn’t optional-it’s life-saving.
Diagnosis: Skin Biopsy Is the Only Way to Know
Emergency rooms see rashes all the time. Most are harmless. But SJS/TEN can be mistaken for staph infections, drug rashes, or even psoriasis. The only way to be sure? A skin biopsy.
Under the microscope, doctors look for full-thickness death of skin cells with almost no inflammation in the deeper layers. That’s the fingerprint of SJS/TEN. Other conditions show lots of immune cells. This one doesn’t. That’s why it’s so dangerous-it looks deceptively quiet until it’s too late.
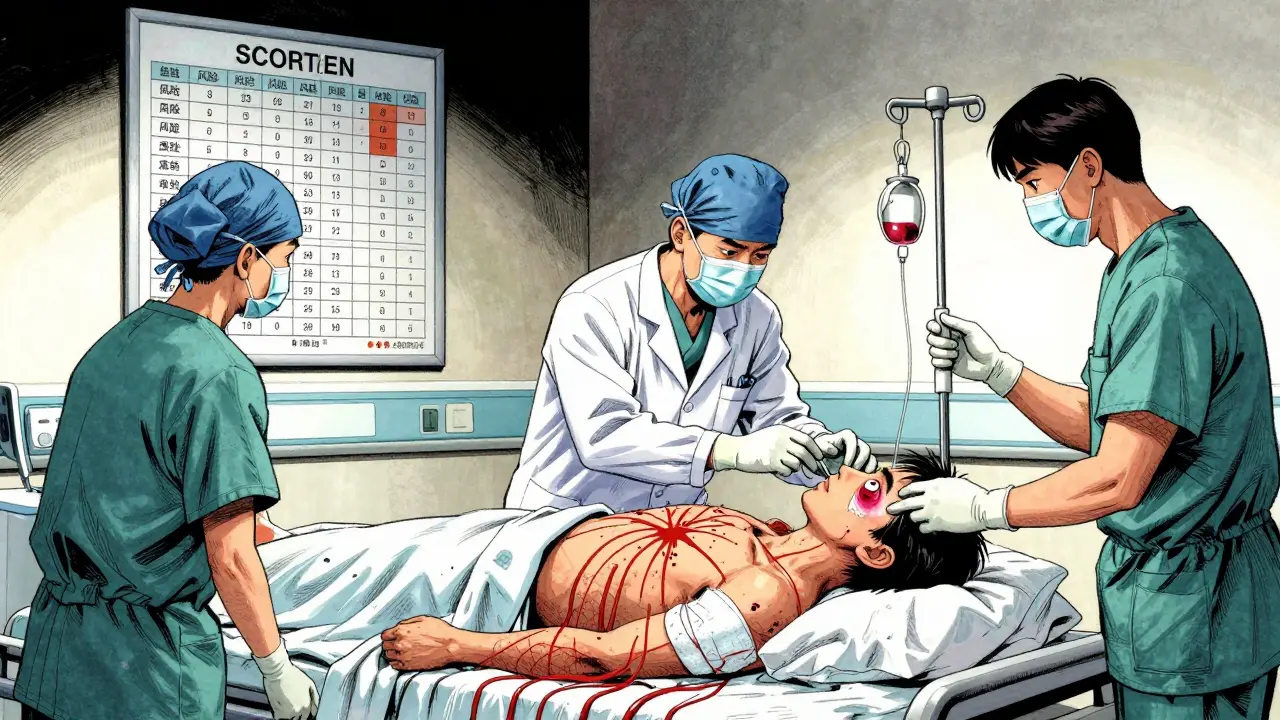
Doctors also use the SCORTEN score to predict survival. It looks at seven things: age over 40, cancer history, heart rate over 120, skin detachment over 10%, high blood sugar, high urea, and low bicarbonate. Each factor adds risk. Three factors? 35% chance of death. Five or more? Nearly 90%. That’s why early diagnosis isn’t just helpful-it’s everything.
What Happens in the Hospital
If SJS/TEN is suspected, you’re not going home. You’re going to a burn unit or ICU. The first rule? Stop every non-essential medication. Every single one. Even if it seems unrelated. You might be taking five pills. One of them is killing you. Figuring out which one takes time, so all are stopped.
Fluid loss is massive. Your skin can’t hold water anymore. You need three to four times your normal fluid intake just to stay alive. IV fluids, electrolytes, nutrition-all delivered through a line. Pain control is critical. These patients describe the pain as worse than childbirth or a major burn.
Wound care is delicate. No sticky bandages. No antiseptics that sting. Just sterile, non-adherent dressings. Your skin is gone. What’s underneath is vulnerable. Infections spread fast. Sepsis is the #1 killer.
Eye care? Daily. Up to 80% of survivors have lasting eye damage. Dryness, scarring, even blindness. Ophthalmologists must be involved from day one to prevent your eyelids from fusing shut.
Treatment: What Works, What Doesn’t
There’s no magic pill. But some treatments show real promise.
IVIG-high-dose antibodies-was once the go-to. But large studies later showed it didn’t lower death rates. So it’s no longer standard.
Corticosteroids? Risky. They suppress your immune system, which sounds good-until you get a deadly infection. Some doctors still use them early, but it’s controversial.
Cyclosporine? This immune modulator showed better results. One 2016 trial cut mortality from 33% to 12.5%. It’s now used in many centers.
Etanercept? A TNF-alpha blocker used for arthritis. In a 2019 study, 12 TEN patients treated within 48 hours had zero deaths. That’s unheard of. It’s not FDA-approved for this, but it’s being used off-label with success.
The future? Drugs that block granulysin, the actual toxin that kills skin cells. Phase II trials start in 2024. That’s the real hope.
What Survivors Live With
Surviving SJS/TEN doesn’t mean you’re back to normal. Sixty to eighty percent of survivors deal with long-term problems.
Your skin? It may be darker or lighter in patches. Scar tissue can form. Nails may grow deformed or fall off.
Your eyes? Dryness, light sensitivity, blurry vision. Many need daily lubricating drops for years. Some need corneal transplants.
Your genitals? Scar tissue can cause painful narrowing of the urethra or vaginal opening. Surgery may be needed.
And then there’s PTSD. Forty percent of survivors develop it. The trauma of being hospitalized, the pain, the fear, the isolation-it sticks. You don’t just heal physically. You heal mentally, too.
Can It Be Prevented?
Yes. And it’s easier than you think.
If you’re prescribed carbamazepine, lamotrigine, or allopurinol-ask for HLA testing. It’s a simple blood test. Results take hours now, not weeks. The FDA approved a point-of-care test for allopurinol in 2022. It’s fast. It’s accurate. It’s cheap.
If you’ve had a bad reaction to any drug before-especially a rash or blistering-never take it again. Tell every doctor. Write it down. Keep a list. Your medical history matters.
And if you ever develop a rash with fever and mouth sores after starting a new drug-go to the ER. Don’t wait. Don’t call your doctor tomorrow. Go now. Early intervention is the only thing that saves lives.
SJS and TEN are rare. But they’re not random. They’re predictable. And with the right knowledge, they can be prevented.


15 Comments
If you’re on carbamazepine or allopurinol and haven’t been tested for HLA-B*15:02 or HLA-B*58:01, ask your doctor why today. This isn’t theoretical-it’s preventable.
It’s wild how medicine still treats these as rare flukes when they’re literally genetic landmines. 🤔 We test for everything else-why not this? Humanity’s got the tools. We just need the will.
My cousin survived TEN after a single dose of ibuprofen. She’s 3 years out. Still needs eye drops daily. No one warned her. No one warned us. This needs to be standard info.
Wow, such a *fascinating* deep dive into the medical-industrial complex’s failure to prioritize genetic screening. I mean, really-why would anyone bother with a $50 test when you can just pray? 😌
From a pathophysiological standpoint, the granulysin-mediated keratinocyte apoptosis cascade is the central mechanistic pivot-this isn't merely an immune dysregulation event, it's a targeted cytolytic cascade triggered by HLA-restricted T-cell activation. The clinical implications are staggering: if we can neutralize granulysin within the 48-hour therapeutic window, we're not just improving survival-we're fundamentally altering disease trajectory. Phase II trials in 2024 might be the first true paradigm shift since ICU management became standard.
SCORTEN score is underutilized. Most ERs don’t even know the parameters. They see a rash, give antihistamines, send them home. That’s malpractice waiting to happen.
My sister got this from a common antibiotic in Nigeria. No testing. No warning. She lost her eyelids. Now she can’t cry. 🙏
Oh wow, so the solution is... *asking your doctor*? Groundbreaking. I bet they just didn’t think of it because they were too busy ignoring the 10,000 other things they’re supposed to do. /s
Let’s be real-this isn’t about medicine. It’s about capitalism. Why test people when you can sell them a $300 pill and then charge $50,000 to patch them back together? The system doesn’t want you alive-it wants you *billed*.
While the author’s intent is laudable, the conflation of correlation with causation in the HLA association data is methodologically unsound. Population-specific allele frequencies do not equate to individual risk profiles without multivariate adjustment. Furthermore, the assertion that "it’s easier than you think" trivializes the logistical and socioeconomic barriers to genetic screening in under-resourced settings.
THIS IS A GLOBALIST PLOT. Why would they push genetic testing? So the WHO can track your DNA and control your meds. They already put fluoride in the water. Now they want your HLA profile. 🚨🇺🇸
My uncle got this from a generic painkiller. He was fine for 6 months. Then-boom. Burn unit for 3 weeks. Now he can’t eat spicy food. Don’t wait. If you’ve had a weird rash after meds? Never take it again. Simple.
STOP. RIGHT. NOW. You’re telling me we’ve known about this for DECADES-and we still don’t have a national mandate? We test for Down syndrome in utero, but not for a 25% mortality risk from a pill? This is criminal negligence.
YOU CAN SAVE A LIFE TODAY. Just ask your doctor for the test. Seriously. Five minutes. One question. That’s it. Don’t wait for a tragedy to make you speak up.
Of course the article ignores the fact that 90% of these cases happen in people who lied about their drug history. You think they’re gonna tell their doctor they took that sketchy Mexican painkiller? This isn’t a medical failure-it’s a behavioral one.
Write a comment