Scleroderma isn't just a skin condition. It’s a systemic autoimmune disease that causes your body to overproduce collagen-turning soft tissues into hardened, scar-like tissue. This isn’t a rare curiosity; it affects about 300,000 people in the U.S. alone, with most diagnoses happening between ages 30 and 50. Women are four times more likely to develop it than men. What starts as cold fingers turning white or blue can, over years, lead to lung scarring, heart damage, and digestive failure. And yet, most people-doctors included-don’t recognize the early signs until it’s too late.
What Happens Inside Your Body With Scleroderma?
Scleroderma, also called systemic sclerosis, doesn’t just attack the skin. It targets your connective tissues-the scaffolding that holds your organs together. The immune system goes haywire, triggering fibroblasts to flood your body with collagen. This isn’t normal healing. It’s uncontrolled scarring. Skin becomes tight, shiny, and hard. Fingers curl inward. Swallowing gets harder. Lungs stiffen like old rubber. The heart struggles to pump. Blood vessels narrow, cutting off circulation.
Almost everyone with systemic scleroderma develops Raynaud’s phenomenon-fingers or toes turning white, then blue, then red when cold or stressed. In 90% of cases, this shows up 5 to 10 years before other symptoms. That’s a critical window. But most patients see three or more doctors over 18 months before someone connects the dots.
Then comes skin thickening, called sclerodactyly. Your fingers lose flexibility. Buttoning a shirt becomes impossible. You start using adaptive tools-jar openers, zipper pulls, grip aids. By the time skin tightens, internal damage may already be underway. Ninety percent of patients have trouble with their digestive tract. Acid reflux isn’t just uncomfortable-it’s constant, damaging the esophagus. Constipation or diarrhea becomes routine. Weight loss follows.
The Two Main Types: Localized vs. Systemic
Not all scleroderma is the same. There are two major forms:
- Localized scleroderma (morphea) affects only patches of skin-sometimes in lines or oval shapes. It doesn’t spread to organs. It’s more common in children and rarely life-threatening.
- Systemic scleroderma is the dangerous kind. It invades internal organs. Two subtypes exist:
Diffuse cutaneous systemic sclerosis hits fast. Skin thickens rapidly over the first 3-5 years. Hands, face, chest, and abdomen tighten. Internal organs follow quickly. About 30-45% of these patients develop heart problems. 80% get lung scarring. This form has the lowest survival rate-only 55-70% live 10 years after diagnosis.
Limited cutaneous systemic sclerosis moves slower. Skin thickening is mostly on fingers, hands, and face. Internal damage comes later. But here’s the catch: even if skin looks stable, the lungs and blood vessels can be silently failing. This is where pulmonary arterial hypertension (PAH) creeps in. It’s the #1 cause of death in scleroderma, responsible for 30-40% of fatalities. Regular echocardiograms are non-negotiable.
How Is It Diagnosed?
There’s no single blood test for scleroderma. Diagnosis is a puzzle made of symptoms, antibodies, and imaging. The first clue? Antinuclear antibodies (ANA). Over 95% of systemic scleroderma patients test positive. But ANA alone isn’t enough-it shows up in lupus, rheumatoid arthritis, and even healthy people.
What matters more are the specific autoantibodies:
- Anti-Scl-70 (Topoisomerase I) - Found in 30-40% of diffuse cases. Strongly linked to lung fibrosis.
- Anti-centromere (ACA) - Seen in 20-40% of limited cases. Lower risk of organ damage, but higher risk of PAH.
- Anti-RNA polymerase III - Present in 15-25%. Signals rapid skin progression and higher cancer risk.
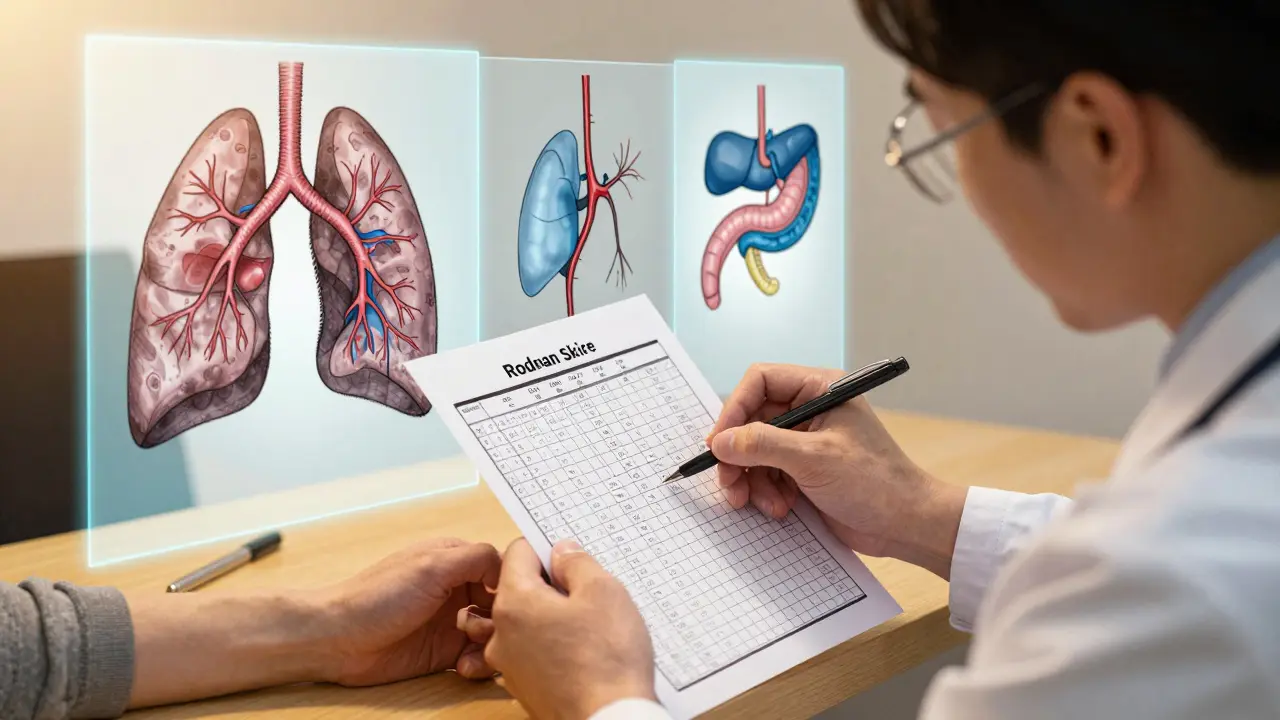
Doctors also use imaging. High-resolution CT scans catch early lung scarring. Echocardiograms screen for heart strain. Pulmonary function tests measure breathing capacity. Skin thickness is scored using the modified Rodnan skin score-a 51-point scale that tracks hardening across 17 body areas. It’s not glamorous, but it’s how progress is measured.
Why Is Treatment So Limited?
There are no FDA-approved drugs that cure scleroderma or stop fibrosis outright. Most treatments are borrowed from other diseases. Immunosuppressants like mycophenolate or cyclophosphamide are used for lung scarring-but they help only 40-50% of patients. A 2023 study showed less than 30% of diffuse scleroderma patients improved their skin score after a year of treatment.
The only FDA-approved drug specifically for scleroderma is tocilizumab, approved in 2021 for interstitial lung disease. It doesn’t fix skin, but it slows lung decline. For Raynaud’s and digital ulcers, iloprost infusions help open blood vessels-but they’re expensive, hard to access, and insurance often denies coverage. For PAH, drugs like ambrisentan or tadalafil are used, same as in pulmonary hypertension from other causes.
What’s frustrating? We treat symptoms, not the root cause. Fibrosis-the scar tissue buildup-is still unstoppable. And that’s why research is exploding. Over 47 active clinical trials are testing new drugs: B-cell depleters, tyrosine kinase inhibitors, anti-fibrotics. One promising approach is autologous stem cell transplant. In the 2023 SCOT trial, half the patients saw major skin improvement lasting over 4 years. It’s risky, but for severe cases, it’s becoming a real option.
Life With Scleroderma: The Daily Reality
Most people don’t realize how much scleroderma steals from daily life. In a 2023 survey of 1,245 patients:
- 78% struggled with hand function-opening jars, turning keys, typing.
- 82% had serious GI issues-reflux, bloating, swallowing pain.
- 70% were too tired to work full-time.
- 60% developed painful digital ulcers that needed weekly wound care.
Patients often need a team: a rheumatologist, pulmonologist, cardiologist, gastroenterologist, and physical therapist. But only 35% of U.S. patients get care at one of the 45 designated scleroderma centers of excellence. The rest rely on general rheumatologists who may have never seen more than a few cases.
Specialized centers like Johns Hopkins, Stanford, and the University of Michigan report better outcomes. Patients who see their team quarterly have fewer hospital visits. They get better education. They’re more likely to catch lung or heart problems early.

What’s Changing in 2026?
There’s real hope now. The Scleroderma Research Foundation committed $15 million in May 2024 to fund fibrosis-targeted therapies. Stanford launched a telemedicine program in January 2024, serving rural patients with monthly virtual visits-and cut hospitalizations by 32% in six months.
A new blood biomarker, serum CXCL4, showed up in the New England Journal of Medicine in March 2024. It may allow diagnosis before skin changes even appear. That’s huge. Earlier detection means earlier intervention.
But the biggest challenge ahead? Aging. As survival rates improve, more patients are living into their 60s and 70s. Now they’re dealing with scleroderma on top of arthritis, diabetes, heart disease. Managing all of it at once is a nightmare for doctors and patients alike.
What You Can Do Now
If you have Raynaud’s, especially if it’s severe or started before age 30, don’t wait. Get tested for ANA and specific antibodies. Track your symptoms: cold triggers, skin changes, swallowing trouble, fatigue. Keep a diary. Bring it to a rheumatologist who specializes in autoimmune diseases-not just any doctor.
Protect your hands. Wear gloves in cold weather. Use hand warmers. Avoid smoking-it tightens blood vessels and makes everything worse.
Manage your stomach. Eat small meals. Don’t lie down after eating. Elevate your head while sleeping. Proton pump inhibitors help, but they’re not a cure.
Find a center. If you’re diagnosed, ask: “Do you treat scleroderma regularly? Do you work with a team?” If the answer is no, push for a referral. Your life depends on it.
Is scleroderma the same as lupus?
No. Lupus causes widespread inflammation and can affect kidneys, brain, and blood cells. Scleroderma is defined by fibrosis-excessive scar tissue buildup in skin and organs. While both are autoimmune and share some symptoms like fatigue and joint pain, scleroderma’s hallmark is hardened skin and internal scarring, not the butterfly rash or kidney flare-ups typical in lupus.
Can scleroderma be cured?
There is no cure yet. But treatments can slow progression, manage symptoms, and improve quality of life. New drugs in clinical trials are targeting the root cause-fibrosis-offering real hope for future breakthroughs. Early diagnosis and specialized care significantly increase survival and function.
Does scleroderma run in families?
It’s not directly inherited like a genetic disease. But having a close relative with an autoimmune condition (like lupus, thyroid disease, or rheumatoid arthritis) slightly increases your risk. Environmental triggers-like exposure to silica dust, solvents, or certain viruses-likely interact with genetic susceptibility to start the disease.
How often should I get lung scans if I have scleroderma?
Annual high-resolution CT scans and pulmonary function tests are standard for all systemic scleroderma patients-even if you feel fine. Lung scarring often develops without symptoms until it’s advanced. Early detection with imaging gives you the best shot at slowing it down with medication.
Are there any new treatments on the horizon?
Yes. Over 40 clinical trials are testing new drugs targeting fibrosis, including B-cell depleters, tyrosine kinase inhibitors, and anti-fibrotic agents. Autologous stem cell transplant has shown long-term skin improvement in severe cases. A blood test for CXCL4 may soon allow diagnosis before symptoms appear. These aren’t just theory-they’re in active human trials.

10 Comments
So let me get this straight-we have a disease that turns your body into a walking mummy, and the best we can do is borrow drugs from other conditions like we're raiding a pharmacy dumpster? 🤦♀️ Meanwhile, the real solution is probably just... stopping the immune system from going full OCD on collagen. But nope, we'll keep patching leaks while the whole house burns down. Classic.
I mean... we're all just bags of water and collagen anyway 😅 But when your skin starts looking like a dried-up grape and your fingers won't uncurl... that's when you realize biology isn't just weird-it's *betraying* you. 🫠
It's terrifying how much of this disease flies under the radar. Raynaud’s is so common people dismiss it as 'just being cold.' But if you're under 30 and your fingers turn blue in the grocery store, that's not a personality quirk-it's your body screaming for attention. The fact that it takes 18 months on average to get diagnosed says more about our medical system than it does about the disease.
You Americans act like this is some unique tragedy. In India, we have people working in silica mines for 12 hours a day with no PPE, and you think *this* is bad? At least you have CT scans and tocilizumab. We have mothers with stiff hands carrying buckets of water on their heads while their lungs fail. Your 'epidemic' is a luxury problem wrapped in a white coat.
Did you know the pharmaceutical companies *want* this disease to stay underdiagnosed? Fewer patients = less pressure to develop real cures. They profit more from lifelong symptom management. That’s why they fund all those 'clinical trials' that just tweak existing drugs. The CXCL4 biomarker? Probably already suppressed. They don’t want early detection-they want lifelong subscribers.
My cousin was diagnosed last year. She started with cold fingers, then couldn't button her shirts. Now she uses a voice-to-text app because typing hurts. She’s not bitter, though. She started a YouTube channel teaching people how to adapt-jar openers, grip gloves, even DIY heated gloves. She turned her nightmare into a mission. That’s the real win here.
The modified Rodnan skin score is one of the most underappreciated tools in rheumatology. 17 body areas, 51 points-measurable, objective, repeatable. It’s not sexy like gene sequencing, but it’s how we know if a treatment is working. We need more metrics like this for chronic diseases. Anecdotes don’t move the needle; data does.
In Nigeria, we say 'the body is a temple, but sometimes the landlord is a thief.' Scleroderma is like your landlord deciding to pour concrete into your lungs and calling it 'upgrades.' You pay rent with your breath, and they charge extra for oxygen. But hey-at least you can still see your toes. Some of us can't even afford to see a doctor.
I JUST FOUND OUT MY BEST FRIEND HAS THIS AND I DIDN'T EVEN KNOW IT WAS A THING?? I THOUGHT SHE WAS JUST BEING LAZY OR STRESSED OR SOMETHING?? SHE'S BEEN WEARING GLOVES IN SUMMER AND I THOUGHT IT WAS A FASHION STATEMENT?? I'M SO SORRY I DIDN'T ASK I'M SUCH A BAD FRIEND 😭
It’s interesting how the disease progression mirrors the frustration of medical discovery. We see the symptoms first-skin, Raynaud’s, GI issues-but the real damage is silent. Like watching a tree rot from the inside while the leaves still look green. That’s why the push for CXCL4 and early biomarkers matters so much. We’re learning to see the rot before the branches fall.
Write a comment