When you have rheumatoid arthritis (RA), knowing how active your disease is isn’t just about how sore your joints feel. It’s about catching hidden inflammation before it destroys your bones and cartilage. That’s why doctors use three key tools: CDAI, DAS28, and imaging. These aren’t optional extras-they’re the backbone of modern RA care. Used together, they help decide if your treatment is working, if it needs to change, or if you’re heading toward remission.
What Is CDAI, and Why Do Doctors Prefer It?
The Clinical Disease Activity Index, or CDAI, is a simple, no-lab-needed score that sums up four things: how many tender joints you have, how many swollen joints, how bad your pain feels on a scale of 0 to 10, and how bad your doctor thinks your disease is on the same scale. Add them all up, and you get a number between 0 and 76. Lower is better.
Here’s what the numbers mean:
- Remission: under 2.8
- Low disease activity: 2.8 to 10
- Moderate: 10 to 22
- High: over 22
Why do over 78% of U.S. rheumatologists use CDAI in most visits? Because it’s fast. It takes less than two minutes. No blood draw. No waiting for lab results. You walk in, your doctor checks your joints, you rate your pain, and you’re done. EHR systems even auto-calculate it. In practices that use it, monitoring frequency jumped from 58% to 89% of visits.
It’s also predictive. Studies show people with high CDAI scores are over four times more likely to develop new joint damage over the next year than those in remission. That’s why the American College of Rheumatology says CDAI should be your first-line tool-especially when labs aren’t ready.
DAS28: The Lab-Dependent Alternative
DAS28 is older and more complex. It uses the same joint counts as CDAI but adds a blood test-either ESR (erythrocyte sedimentation rate) or CRP (C-reactive protein). There are two versions: DAS28-ESR and DAS28-CRP. The formula looks intimidating, but the goal is simple: measure inflammation more precisely.
Its thresholds are slightly tighter:
- Remission: under 2.6
- Low: 2.6 to 3.2
- Moderate: 3.2 to 5.1
- High: over 5.1
But here’s the catch: labs take time. In 68% of cases, the CRP result comes back after the appointment. That means doctors often make treatment decisions based on incomplete data. One rheumatologist told me, “I’ll say ‘let’s up the dose’ and then get the CRP back and realize it was normal. Now I’m stuck.”
DAS28 is still widely used in Europe, where 68% of practices rely on it. But in the U.S., it’s losing ground-not because it’s inaccurate, but because it’s slower. If you’re getting frequent blood work anyway, DAS28-CRP gives you extra insight into how much inflammation is brewing under the surface. But if you’re trying to make a quick call during a 15-minute visit? CDAI wins.
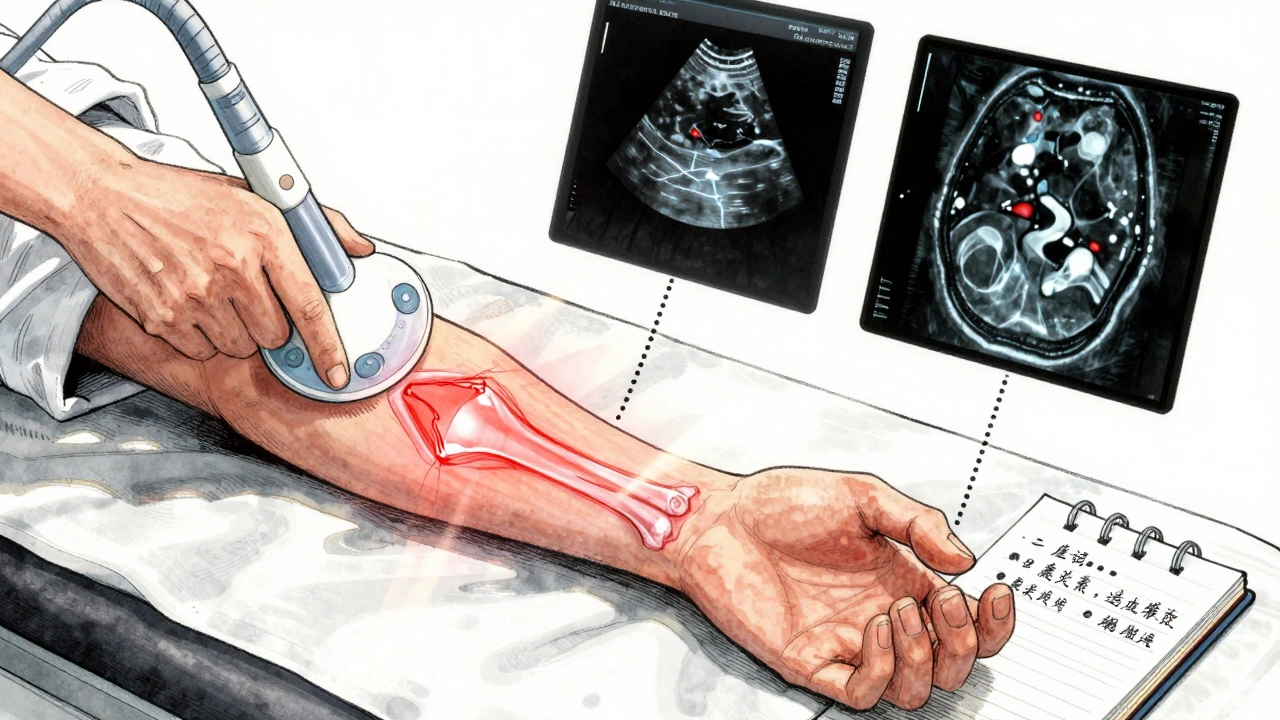
Imaging: Seeing What Your Eyes Can’t
Even if your CDAI or DAS28 looks good, your joints might still be quietly breaking down. That’s where imaging comes in.
There are three main types:
- Conventional X-rays: The gold standard for tracking bone damage. They show erosions and joint space narrowing. But they’re blind to early inflammation. It takes 6 to 12 months of damage before X-rays catch it.
- Ultrasound: This is the game-changer. It shows swollen synovium (the lining of the joint) and active blood flow (power Doppler) in real time. It’s 85% better at spotting synovitis than a physical exam alone. And it’s cheap-around $150 per scan. Many rheumatologists now do it right in the office. In 22% of cases, ultrasound changes the treatment plan when clinical exam says “no change needed.”
- MRI: The most sensitive tool. It picks up bone edema (osteitis)-inflammation inside the bone-up to a year before X-rays show damage. Studies show 89% of people with bone edema will develop erosions within a year. But MRI costs about $1,200 and isn’t always covered unless you’re at high risk.
Doctors don’t scan everyone every time. They use imaging strategically. If your CDAI is low but you still have pain, they might order an ultrasound to check for hidden synovitis. If your joints are crumbling but your scores are low, an MRI can tell you if inflammation is still active underneath.
How Do These Tools Compare in Real Life?
A 2023 study of nearly 4,000 RA patients found CDAI matched doctors’ overall clinical judgment better than any other tool-84% correlation. DAS28-CRP came in at 79%. Patient-reported scores like RAPID-3? Only 39%. Why? Because pain and fatigue don’t always match what’s happening inside the joints.
There’s another problem: discordance. In one Brazilian study, 33% of patients rated their disease as worse than their doctor did. That’s not just disagreement-it’s a risk. If you say you’re in high pain and your doctor doesn’t see swelling, they might hold off on treatment. But if you’re hiding inflammation, you’re still at risk for damage.
And here’s the flip side: sometimes, imaging shows damage even when scores are low. In 35% of cases, there’s a mismatch between what the numbers say and what the images show. That’s why doctors don’t rely on one tool alone. They triangulate.
What’s the Best Approach for You?
There’s no one-size-fits-all. But here’s what most experts recommend:
- Start with CDAI at every visit. It’s fast, accurate, and tied to real outcomes.
- If you’re in remission or low disease activity, get an X-ray once a year. If you’re stable, every 2 years may be enough.
- If you have ongoing symptoms despite low scores, ask for ultrasound. It’s non-invasive, affordable, and can reveal hidden inflammation.
- Only consider MRI if you’re at high risk-early disease, high autoantibodies, or rapid progression. It’s not for routine use.
Some new tools are emerging. Apps like RheumaTrack let you log symptoms daily. Wearable sensors track joint movement and fatigue. AI software can now analyze ultrasound images automatically, matching expert readings 88% of the time. By 2027, half of RA monitoring might include continuous remote data.
But for now, the basics still work best: a good joint count, a clear picture of your pain, and the right image at the right time. You’re not just managing symptoms-you’re protecting your future mobility.
What Happens If You Don’t Monitor?
Without regular monitoring, RA doesn’t just stay the same-it gets worse. Studies show that using treat-to-target strategies with these tools cuts joint damage progression by 30% to 50%. That means fewer surgeries, less disability, and more years of being able to open jars, hold your grandkids, or walk without pain.
Yet, 22% of U.S. rheumatology practices still don’t use standardized tools. Many are in rural areas, where access to training and tech is limited. If you’re seeing a doctor who never checks your joint count or doesn’t order imaging, ask why. You deserve a plan that’s based on data, not guesswork.
What You Can Do
- Know your scores. Ask your doctor for your latest CDAI or DAS28 number. Write it down.
- Track your own symptoms. Use a notebook or app to record pain, stiffness, and fatigue between visits.
- Ask about ultrasound if you’re still having symptoms. Don’t assume low scores mean everything’s fine.
- Push back if you’re being pushed into unnecessary MRIs. Ask: “Is this based on my risk, or just routine?”
- Bring your own data. If you’ve noticed more swelling in your knuckles or worse morning stiffness, say so. Your input matters.
RA isn’t just about pills. It’s about tracking, adjusting, and staying ahead. The tools exist. The evidence is clear. The goal isn’t just to feel better today-it’s to keep your joints strong for decades to come.

15 Comments
CDAI? More like CDAI - Corporate Doctor's Automated Illusion. They don't care if you're in pain. They care if the algorithm says 'low activity'.
Next thing you know, they'll replace doctors with chatbots that read joint counts from a phone camera.
This is what happens when Western medicine thinks numbers replace human experience. My aunt in Johannesburg has RA and no access to any of this. Her doctor looks at her hands and says 'keep moving'. She’s still walking at 72. You think a score matters when you’re hungry?
Yessss this is so important!! 💪 I’ve been tracking my CDAI for 2 years now and honestly? It’s been my lifeline. My doc actually listens when I say 'my score’s creeping up' 😊 You’re not just a number-you’re a person with a story. Keep advocating!! 🙌
The entire paradigm of RA management is a grotesque caricature of clinical science reduced to bureaucratic checkboxes
One must question whether the obsession with quantifiable metrics serves the patient or the insurance industry
When did we stop trusting intuition and start trusting spreadsheets
CRP levels are meaningless if the patient is crying in the waiting room
Yet the system rewards compliance not compassion
CDAI is a scam. They use it because it’s cheap and the drug companies love it. You think they want you in remission? Nah. They want you on biologics forever. Ultrasound? That’s just the gateway to MRI. And MRI? That’s how they upsell you into clinical trials. Wake up.
Lmao CDAI? More like CDAI - Controlled Doctor's AI lie. My doc said my score was low so he cut my meds. Two weeks later my wrist looked like a deformed potato. Turns out the CRP was normal but my synovitis was screaming. They dont wanna see what they cant measure.
Thank you for this comprehensive overview. As a physician from India, I can confirm that access to these tools varies drastically. In rural clinics, we rely on clinical judgment alone. Yet even then, the principles remain: observe, listen, and act with care. The tools are aids-not replacements-for human wisdom.
I’ve been in remission for 8 years. No meds. No scans. Just yoga, turmeric, and silence. You think you need all this tech? You just need to stop treating your body like a broken machine. The system wants you dependent. Don’t be a sheep.
There’s beauty in the balance. CDAI gives speed. DAS28 gives depth. Imaging gives truth. But none of it matters if the doctor doesn’t sit down, look you in the eye, and ask: 'How are you really doing?' The tools are good. The system? Still learning how to use them.
CDAI is just a fancy way of saying 'guess how bad you feel' and then pretending it's science. My score was low last month so they stopped my methotrexate. Now I can't button my shirt. Guess what? My pain didn't disappear. Just the paperwork.
I remember when my rheumatologist said 'your DAS28 is fine'... then I had a heart attack two weeks later. Turns out inflammation doesn't just live in your joints. It's in your arteries. Your blood vessels. Your soul. They monitor joints. But who monitors the whole person?
The entire framework of RA management is a monument to the cult of quantification where human suffering is reduced to a decimal point on a spreadsheet and the only thing more dangerous than the disease is the system that claims to cure it
They measure joints but ignore the grief
They track CRP but silence the voice
They call it precision medicine when it’s just precision control
I must respectfully challenge the assertion that CDAI is superior to DAS28. While speed is advantageous, the omission of objective inflammatory markers fundamentally undermines clinical accuracy. In high-risk patients, this may constitute a breach of the standard of care.
I got an ultrasound last month. Doc said 'nothing's there.' I said 'but my knuckles burn.' He did another scan. Found synovitis. Turned out I was right. Trust yourself. Even if the score says you're fine.
This is why America’s healthcare is broken. You need a $1200 MRI to prove you’re in pain? Meanwhile, China gives free acupuncture and herbal packs. We’re outsourcing our humanity to algorithms while the rest of the world heals with touch.
Write a comment