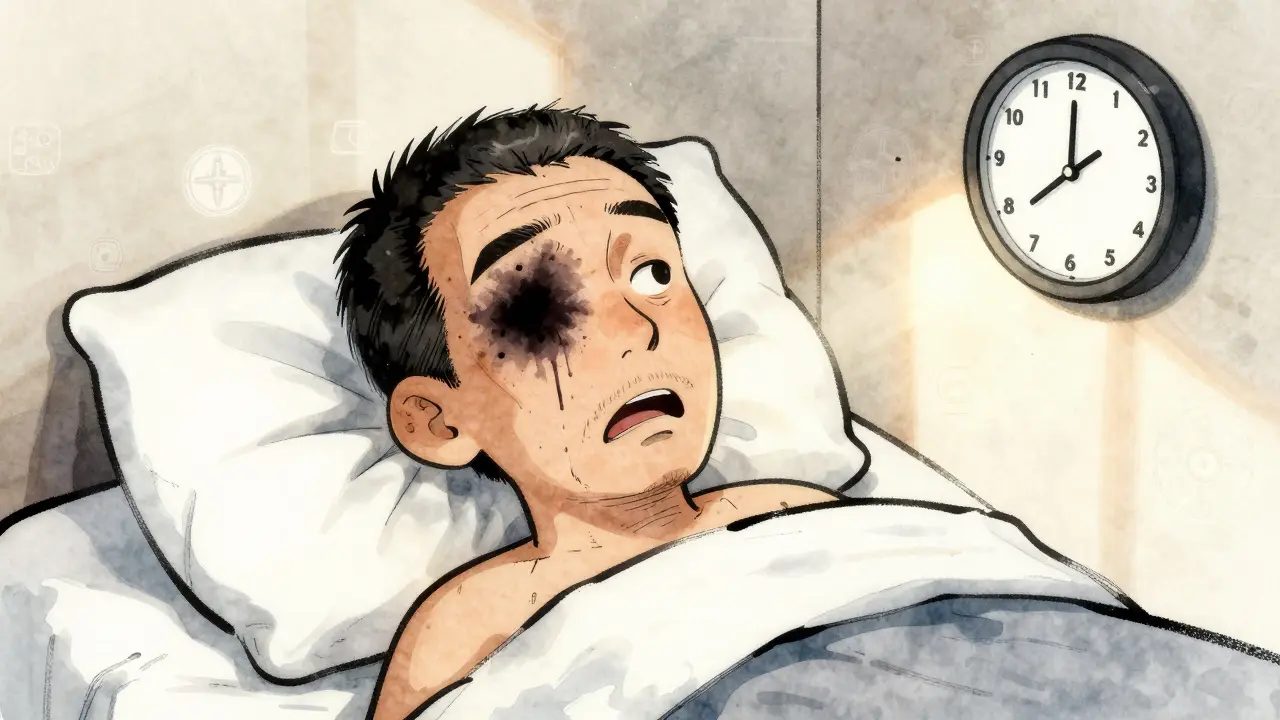
When you wake up one morning and notice your vision is blurry or dark in one eye-with no pain, no redness, no warning-it’s not just a tired eye. It could be retinal vein occlusion (RVO), a sudden blockage in the tiny veins that drain blood from the retina. This isn’t rare. Around 16 million people worldwide have it, and it’s one of the top causes of sudden vision loss after diabetic eye disease and age-related macular degeneration. The good news? We can treat it. The challenge? It often comes with lifelong management and repeated injections.
What Exactly Is Retinal Vein Occlusion?
Your retina is like the film in a camera-it captures light and sends signals to your brain. Blood flows into the retina through arteries and drains out through veins. When one of those veins gets blocked, blood and fluid leak into the retina, swelling the macula (the center part responsible for sharp vision). That’s macular edema, and it’s what blurs your sight. There are two main types:- Central Retinal Vein Occlusion (CRVO): The main vein behind the eye is blocked. This affects the whole retina and usually causes more severe vision loss.
- Branch Retinal Vein Occlusion (BRVO): A smaller branch vein is blocked, often where an artery crosses over it and squeezes the vein. Vision loss is usually partial, like a dark spot in one area of your vision.
Neither type causes pain. That’s why many people ignore early symptoms-until they realize they can’t read the clock or recognize faces.
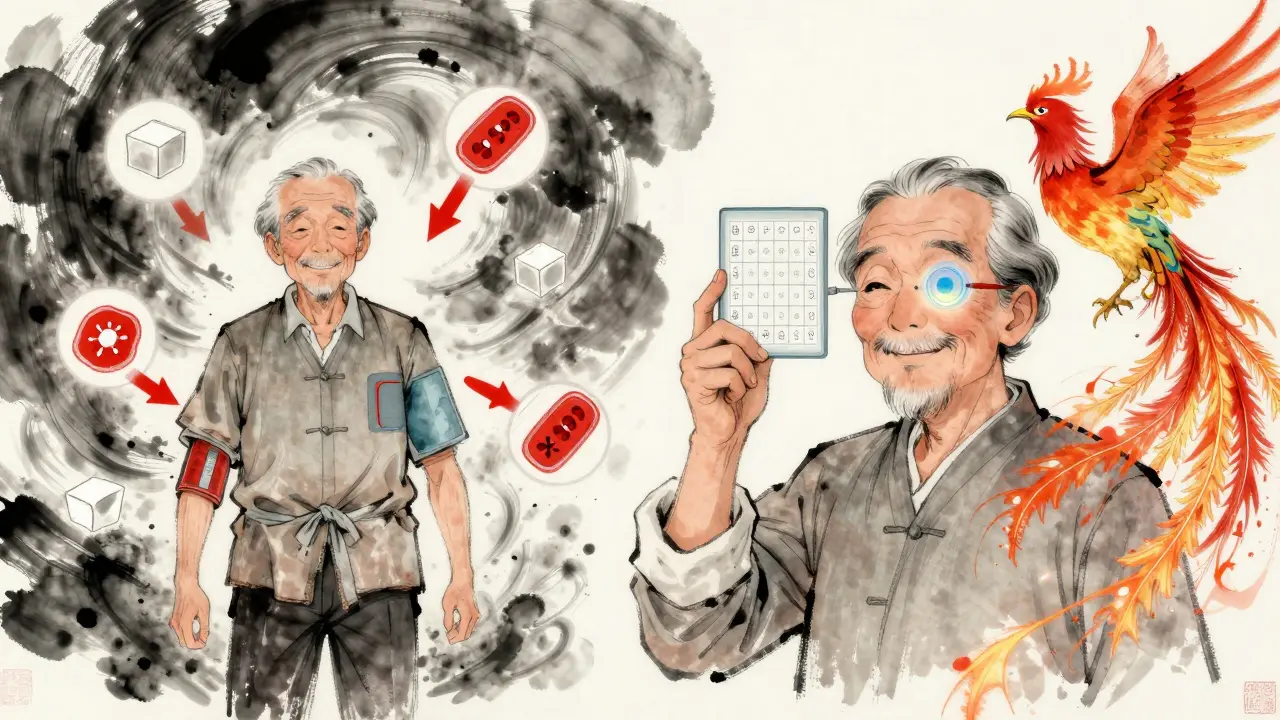
Who’s at Risk? The Real Risk Factors Behind RVO
RVO doesn’t come out of nowhere. It’s almost always tied to underlying problems in your blood vessels. Age is the biggest factor: over 90% of CRVO cases happen in people over 55, and more than half of all cases occur after age 65. But it’s not just older adults-5 to 10% of cases strike people under 45. Here’s what actually increases your risk:- High blood pressure: Present in up to 73% of CRVO patients over 50. Uncontrolled hypertension is the number one driver of vein blockages.
- Diabetes: Affects about 10% of RVO patients over 50. Poorly controlled blood sugar damages blood vessel walls, making them more likely to clot.
- High cholesterol: Total cholesterol above 6.5 mmol/L is found in 35% of RVO patients, regardless of age. Hardened arteries from plaque buildup are a direct cause.
- Glaucoma: High pressure inside the eye, especially near the optic nerve, can compress the retinal vein and trigger a blockage.
- Smoking: Found in 25-30% of cases. Smoking thickens blood and damages vessel linings.
- Obesity and inactivity: Both contribute to poor circulation and higher clotting risk.
- Oral contraceptives: In women under 45, this is the most common link to CRVO. The hormones can make blood more likely to clot.
- Blood disorders: Conditions like polycythemia vera, multiple myeloma, or inherited clotting disorders (like Factor V Leiden) are rare but serious causes, especially in younger patients.
Many people with RVO have two or three of these risk factors. That’s why treating RVO isn’t just about the eye-it’s about your whole cardiovascular system.
The Main Treatment: Injections Into the Eye
There’s no surgery to unblock the vein. Instead, doctors treat the damage it causes-mainly macular edema. The gold standard? Injections directly into the eye. Three types of injections are used:- Anti-VEGF drugs: These block a protein called VEGF that causes leaking and swelling. The most common are:
- Ranibizumab (Lucentis): FDA-approved for RVO since 2010.
- Aflibercept (Eylea): Approved in 2012. Often more effective in severe cases.
- Bevacizumab (Avastin): Originally a cancer drug, used off-label. Costs about $50 per dose, compared to $2,000 for the others.
- Corticosteroid implants: Like Ozurdex, a tiny biodegradable pellet that releases dexamethasone over months. Used when anti-VEGF doesn’t work well enough.
How do these work? Clinical trials show clear results:
- In the BRAVO trial, patients on ranibizumab gained an average of 16.6 letters on the eye chart after a year-nearly double the improvement of those getting fake injections.
- Aflibercept in the COPERNICUS trial improved vision by 18.3 letters on average.
- Ozurdex helped 27.7% of CRVO patients gain 15 or more letters of vision, compared to just 12.9% with placebo.
Most patients start with monthly injections until the swelling goes down. Then, they switch to “as needed” based on follow-up scans. In real life, people need 8 to 12 injections a year to keep vision stable.
How Do Doctors Decide Which Injection to Use?
There’s no single answer. It depends on the patient.- For patients with very poor vision at diagnosis (worse than 20/200): Some retina specialists start with Ozurdex because steroids can reduce swelling faster in severe cases.
- For patients with better baseline vision: Anti-VEGF drugs like aflibercept usually give better long-term results.
- For cost-conscious patients: Bevacizumab is widely used in safety-net clinics. Studies show it’s nearly as effective as the more expensive options.
- For patients who can’t handle monthly visits: Ozurdex lasts 3-6 months, so fewer visits are needed.
But steroids come with trade-offs. About 60-70% of patients who get Ozurdex develop cataracts faster. One in three get elevated eye pressure, which may need drops or surgery. That’s why anti-VEGF is still the first choice for most.
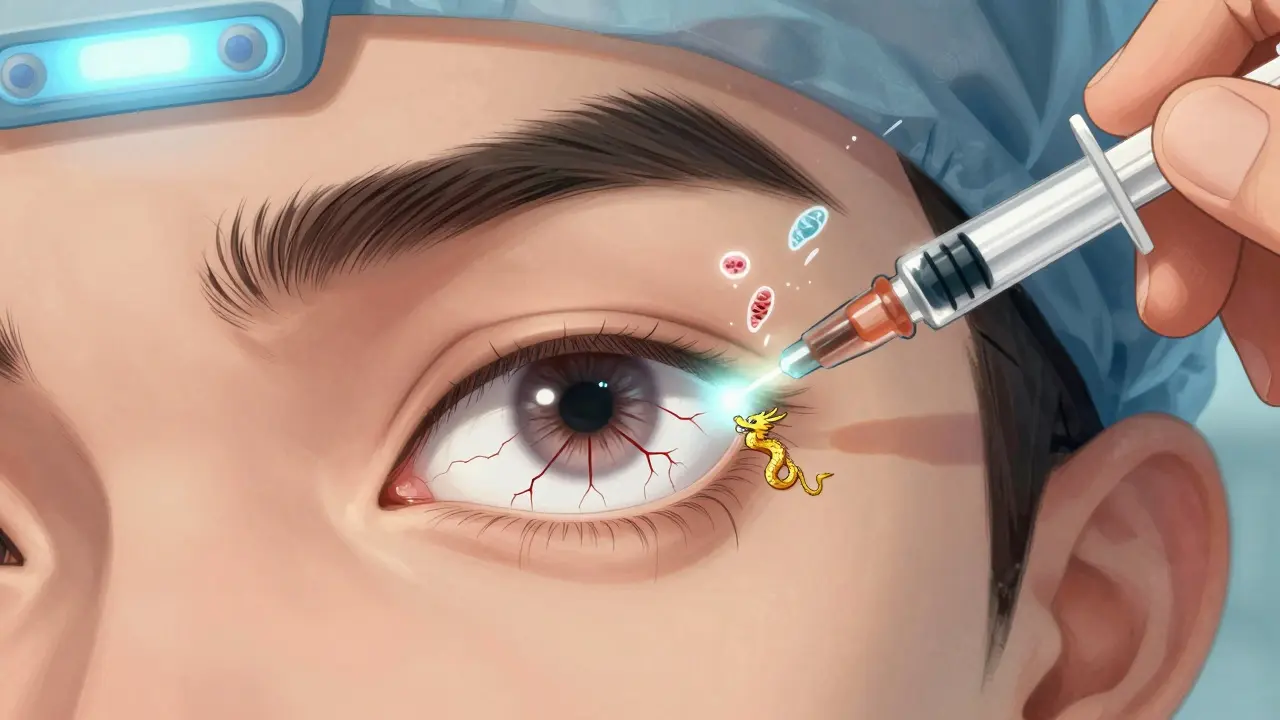
What Happens During an Eye Injection?
It sounds scary-but it’s quick and mostly painless.- You’ll get numbing drops.
- Your eye is cleaned with iodine solution to prevent infection.
- A small device holds your eyelid open.
- The doctor injects the medicine through the white part of your eye, just behind the iris.
- The whole thing takes 5-7 minutes.
Afterward, you might see floaters or have a red spot on the white of your eye. That’s normal-about 1 in 3 people get a small bleed. Serious infections (endophthalmitis) are rare: only 0.02% to 0.1% of injections cause them.
Most people feel pressure, not pain. But anxiety before the shot is common. One patient on Reddit said, “My heart races every time. I know it’s routine, but I still feel like I’m about to get stabbed.”
Real Patient Experiences: Successes and Struggles
Not every story ends with perfect vision.- “RetinaWarrior42,” 62: “After my CRVO, I got Lucentis every month. By month 4, I went from 20/200 to 20/60. But $150 per injection? On a fixed income, it’s a nightmare.”
- “GlaucomaSurvivor”: “I tried 8 Avastin shots with no change. Then I got Ozurdex. Ten lines of vision back. Worth every penny.”
- “MaculaMama”: “After 18 months of shots, I got so anxious I started skipping appointments. My vision kept improving, but I couldn’t face another needle.”
A 2022 survey of 1,247 RVO patients found 78% saw real vision improvement with anti-VEGF therapy. But 63% said cost was a burden, and 41% felt “treatment fatigue”-the emotional toll of endless doctor visits.
What’s New in RVO Treatment?
The future is moving away from monthly shots.- Treat-and-extend protocols: Start monthly, then stretch the time between shots if vision stays stable. One 2023 study showed this cuts injection frequency by 30% with no loss of results.
- Port Delivery System (Susvimo): A tiny implant that refills the eye with ranibizumab every 6 months. Approved for macular degeneration, now being tested for RVO.
- Gene therapy (RGX-314): A one-time injection that teaches your eye to make its own anti-VEGF protein. In early trials, it’s shown promise for lasting effects.
- OPT-302: A new drug that blocks a different VEGF protein. Used with aflibercept, it’s helping patients who didn’t respond to standard treatment.
Doctors are also using advanced scans like OCT angiography to predict who will respond best to which treatment. This isn’t science fiction-it’s happening now.
What You Can Do Now
If you’ve been diagnosed with RVO:- Follow up with your retina specialist regularly-even if your vision seems fine.
- Control your blood pressure, blood sugar, and cholesterol. Medications and lifestyle changes matter as much as the injections.
- Ask about cost-saving options like bevacizumab if you’re uninsured or underinsured.
- Don’t skip appointments because you’re scared. The procedure is safer than most people think.
- Track your vision at home with an Amsler grid. If lines look wavy or missing, call your doctor.
If you’re over 50 and have high blood pressure or diabetes, get a dilated eye exam every year. RVO often has no warning signs. Early detection means earlier treatment-and better vision outcomes.
Can retinal vein occlusion be cured?
No, RVO cannot be cured. The blockage stays. But with treatment, the swelling and leakage can be controlled, and vision can improve or stabilize. Most people need ongoing treatment to maintain their sight.
How long do injections last?
Anti-VEGF injections (like Lucentis or Eylea) work for about 4 to 6 weeks. That’s why monthly shots are common at first. The Ozurdex implant lasts 3 to 6 months and slowly releases steroid medicine.
Are eye injections dangerous?
Serious complications are rare. The biggest risks are infection (0.02-0.1% of cases), increased eye pressure (especially with steroids), and cataracts. Minor issues like redness, floaters, or a small bleed on the white of the eye are common and harmless.
Can I drive after an eye injection?
Not right away. Your vision will be blurry for a few hours, and your pupil will be dilated. You’ll need someone to drive you home. Most people can drive again the next day.
Will I go blind from RVO?
Without treatment, yes-up to 50% of untreated CRVO patients lose significant vision. With timely injections, 30-40% of patients reach 20/40 vision or better. Early treatment is the key to saving sight.
Why do I need so many injections?
The swelling keeps coming back because the underlying vein blockage hasn’t been fixed. The injections don’t unblock the vein-they stop the fluid leak. Once the leak stops, the swelling goes down. But if you stop treatment, the leak returns. That’s why it’s a long-term management plan, not a one-time fix.
Can I use cheaper generic versions of the drugs?
Bevacizumab (Avastin) is a generic version of ranibizumab and is used off-label for RVO. It’s about 40 times cheaper and just as effective in most cases. Many clinics use it, especially for patients with limited insurance coverage. Ask your doctor if it’s right for you.

13 Comments
So basically my eye is a clogged sink and the doctor is just pouring drain cleaner into it? Got it. I’ll bring snacks to my next appointment.
This is the kind of post that makes me feel seen. I’ve had BRVO for 3 years. The injections are brutal, but I can still read my grandkids’ drawings. Worth every needle.
Ah yes, the modern miracle: injecting cancer drugs into your eyeball because capitalism couldn’t be bothered to fix the root cause. We treat symptoms like they’re gods and ignore the fact that we’re all just meat sacks with bad blood pressure. Philosophical, no?
Been there done that. Got the floaters the red spot the anxiety the $2000 bill. Still can see my dog’s face. That’s the win
I know people are scared of injections but honestly the fear is way worse than the thing itself. I used to cry before every one. Now I just listen to hip hop and count to three. It’s over before you know it.
You people are so lucky you even have access to these treatments. In India my cousin got diagnosed with CRVO and the local clinic said ‘come back in 6 months’ and then he disappeared. No one even asked if he had insurance.
The part about Avastin being just as good as Lucentis but 40x cheaper needs to be shouted from the rooftops. Why are we still pretending these drugs are all the same when the cost difference is insane
Let me guess. You’re one of those people who thinks if you just ‘eat clean’ and ‘meditate’ you can reverse RVO. Newsflash: your kale smoothie isn’t unblocking a vein. Stop giving unsolicited advice to people who are already drowning.
I want to thank the author for including the patient stories. That’s what makes this real. Not the stats. Not the drug names. The person who skipped appointments because they were scared. The one who cried in the waiting room. That’s the truth. And it matters.
I got my first injection last week. I thought I’d be terrified. I wasn’t. I was just… tired. Tired of being scared. Tired of wondering if I’d ever see my wedding photo clearly again. The needle didn’t hurt. The silence after the shot did.
its like the body is just giving up and the doctors are like oh we can fix this with magic juice but really we just dont know how to fix the real problem which is our entire system is broken and we are all just waiting to die anyway
As someone who moved from India to the US, I can tell you the difference in care is night and day. But even here, I had to fight for a referral. If you’re over 50 and diabetic? Don’t wait for symptoms. Get checked. Seriously.
I’m just glad I found this. I’ve been avoiding the doctor for months. Now I know I’m not alone. Thanks.
Write a comment