Clozapine ANC Monitoring Timeline Calculator
This calculator shows the current ANC monitoring schedule based on how long you've been on clozapine. The FDA removed the mandatory REMS program on February 24, 2025, but ANC monitoring remains critical for safety.
Important: The FDA removed the mandatory REMS program, but your doctor should still follow the ANC monitoring schedule. Do not skip blood tests.
The FDA removed the mandatory REMS for clozapine on February 24, 2025. That means pharmacies no longer need to check a government database before filling a clozapine prescription. No more waiting for patient enrollment codes. No more monthly paperwork from clinics. No more locked-out prescribers because their certification expired. This isn’t a relaxation of safety-it’s a recognition that doctors and patients have been doing the right thing all along.
Why Was Clozapine Locked Down in the First Place?
Clozapine is one of the most effective medications for treatment-resistant schizophrenia. For people who haven’t responded to two or more antipsychotics, clozapine can mean the difference between living at home and staying in a hospital. But it carries a rare, serious risk: severe neutropenia, a drop in white blood cells that can leave the body defenseless against infection. In the 1990s, a small number of patients died from this. The FDA responded by creating the Clozapine Risk Evaluation and Mitigation Strategy (REMS) in 2015. It turned prescribing clozapine into a bureaucratic maze.Under the old system, every prescriber had to get certified. Every pharmacy had to be certified. Every patient had to enroll. And every month, clinics had to submit a form with the patient’s latest absolute neutrophil count (ANC) blood test result. If the form wasn’t submitted, the pharmacy couldn’t dispense the medication-even if the patient had been on clozapine for five years with perfect ANC numbers.
How ANC Monitoring Actually Worked
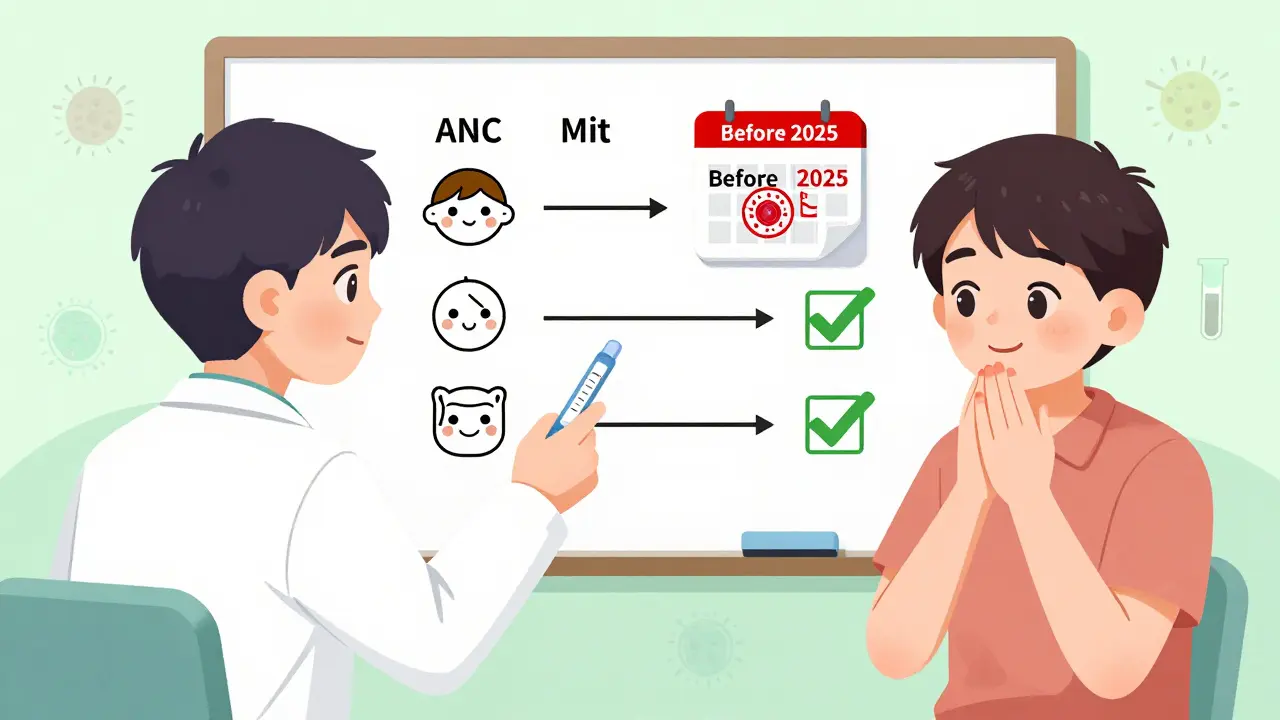
ANC stands for Absolute Neutrophil Count. It’s a simple blood test that measures the number of infection-fighting white blood cells. The old REMS program followed strict timing rules based on how long someone had been on clozapine:- Before starting: Baseline ANC needed to be ≥1500/μL (or ≥1000/μL for people with benign ethnic neutropenia).
- Weeks 1-18: Weekly blood tests.
- Months 6-12: Every two weeks if ANC stayed normal.
- After 12 months: Monthly tests, using shared decision-making with the patient.
These timelines weren’t random. Data from the U.S. Department of Veterans Affairs and the FDA’s own Sentinel System showed the highest risk of neutropenia was in the first 18 weeks. After that, the risk dropped-but never vanished. Even after five years, a tiny percentage of patients still developed low neutrophils. That’s why monitoring didn’t stop. It just became less frequent.
Why the FDA Changed Its Mind
The FDA didn’t remove the REMS because they thought clozapine was safe. They removed it because the system wasn’t working the way it was supposed to.Studies showed that 92% of prescribers were already following the ANC monitoring guidelines-without being forced to. A 2022 survey of psychiatrists found that 84% checked ANC at the right intervals, even when no one was watching. Clinics in rural areas, where access to care was already hard, were dropping patients from clozapine because they couldn’t keep up with the paperwork. One clinic in Nebraska stopped prescribing clozapine entirely because their staff spent over 15 hours a month just filing REMS forms.
Patients were suffering, too. The National Alliance on Mental Illness reported that 30% of people who needed clozapine faced delays of weeks or even months because of REMS. Some gave up. Others switched to less effective drugs that didn’t work as well but were easier to get.
The FDA looked at the real-world data-adverse event reports, pharmacy logs, hospital records-and concluded that the mandatory system wasn’t preventing harm. It was just creating friction. Doctors knew the risk. Patients knew the importance of blood tests. The system wasn’t adding safety-it was adding stress.
What’s Different Now?
As of February 24, 2025:- Prescribers no longer need to be certified by the Clozapine REMS program.
- Pharmacies no longer need to verify patient enrollment or submit ANC results to a federal database.
- Patient enrollment in the REMS portal is no longer required.
- Monthly Patient Status Forms are gone.
- Telecommunication verification (the old “switch system”) is no longer an option-because it’s no longer needed.
But here’s what hasn’t changed:
- The FDA’s Boxed Warning about severe neutropenia is still on every clozapine bottle.
- The prescribing information from Novartis still recommends the same ANC monitoring schedule.
- Clinicians are still expected to monitor ANC weekly for the first 6 months, then less frequently.
- The risk of neutropenia hasn’t disappeared. It’s still about 0.8% over a patient’s lifetime on clozapine.
The FDA is now trusting doctors to use their judgment-just like they do with warfarin, lithium, or methotrexate. Those drugs also carry serious risks. But we don’t force doctors to log every lab result into a federal system. We trust their training.
What This Means for Patients
If you’re starting clozapine, you’ll still need blood tests. You’ll still need to get your ANC checked every week for the first 6 months. Your doctor will still tell you to come in for blood work. But now, you won’t have to wait for a pharmacy to call in a code. You won’t have to beg your clinic to submit a form. You won’t get turned away because the REMS website was down.For people who’ve been on clozapine for years, this means no more annual re-enrollment hassles. No more panic when your certification expires. No more being locked out because your clinic forgot to renew their pharmacy license.
One patient in Ohio told her psychiatrist: “I waited three weeks last year because the REMS portal said my ANC was ‘pending review.’ I had to go without my medicine. I almost relapsed. This time, I got my script the same day.”
What This Means for Doctors and Pharmacies
For prescribers, it’s a relief. No more logging into a separate portal. No more training renewals every two years. No more audit letters. No more explaining to patients why they can’t get their medication even though their blood work is fine.Pharmacies no longer need to dedicate staff to REMS verification. A 2022 survey found that independent pharmacies spent 10-15 extra minutes per clozapine prescription just to check the REMS system. That adds up. One pharmacy in Montana reported they were turning away 2-3 clozapine prescriptions a week because their staff didn’t have time to handle the paperwork. Now, they can fill the script like any other.
But this doesn’t mean clozapine is now “easy.” It still requires vigilance. The American Society of Health-System Pharmacists is rolling out updated guidelines in Q3 2025 to remind clinicians that ANC monitoring is still the standard of care. The FDA is watching through its Sentinel System, tracking neutropenia cases in real time. If something changes-like a spike in severe neutropenia cases-they’ll act.

Why This Matters Beyond Clozapine
The removal of the clozapine REMS is a turning point for how the FDA handles drug safety. For decades, the agency’s go-to answer for any risk was “add a REMS.” Thalidomide? REMS. Isotretinoin? REMS. Even drugs with low risk got them. But clozapine is different. The FDA finally said: “We’ve been overprotecting this drug. The people who use it and prescribe it know how to manage the risk. Let’s trust them.”This sets a precedent. Other drugs with complex safety profiles-like lithium for bipolar disorder or valproate for epilepsy-could see similar changes in the future. If the data shows that clinicians are already doing the right thing, why force them through a bureaucracy?
What’s Next?
Manufacturers are updating clozapine labels to remove all references to the REMS program. By mid-2025, every bottle of clozapine sold in the U.S. will have new prescribing information that says ANC monitoring is recommended-but not mandated.Industry analysts expect clozapine use to jump 25-30% over the next two years. Right now, only about 12% of people with treatment-resistant schizophrenia in the U.S. get clozapine. That’s not because it doesn’t work. It’s because the system made it too hard.
The goal now isn’t to control access. It’s to remove barriers so the right people can get the right medicine-without being treated like criminals for needing a life-changing drug.
What Patients Should Do Now
If you’re on clozapine:- Keep getting your ANC blood tests as scheduled. Don’t skip them.
- Ask your doctor if they’re still following the same monitoring schedule. They should be.
- If you’re starting clozapine, expect weekly blood work for the first 6 months. That hasn’t changed.
- If your pharmacy says they can’t fill your prescription because of “REMS,” they’re wrong. Tell them the program ended in February 2025.
If you’ve been told you’re not a candidate for clozapine because of “the REMS program,” ask again. The barrier is gone. The only thing standing in your way now is whether your doctor believes it’s right for you.
Is clozapine still dangerous?
Yes, clozapine still carries a risk of severe neutropenia, especially in the first six months of treatment. But the risk is low-about 0.8% over a patient’s lifetime-and it’s well understood. The FDA removed the mandatory REMS because doctors have been monitoring patients properly for years. The Boxed Warning remains on all clozapine labels to remind everyone of this risk.
Do I still need to get blood tests for clozapine?
Yes. Even though the FDA no longer requires you to report your ANC results, your doctor should still order weekly blood tests for the first 6 months, then biweekly for months 6-12, and monthly after that. This isn’t a government rule anymore-it’s medical best practice. Skipping tests increases your risk of missing early signs of neutropenia.
Can my pharmacy refuse to fill my clozapine prescription now?
No. Pharmacies can no longer require you to be enrolled in the REMS program or submit ANC results to a federal database. If they say they can’t fill your prescription because of REMS, they’re using outdated rules. Tell them the program ended on February 24, 2025. If they still refuse, ask to speak to the pharmacist-in-charge or contact your prescriber.
Why did the FDA wait until 2025 to remove the REMS?
The FDA began reviewing the REMS in 2024 after years of pressure from clinicians and patient groups. They analyzed real-world data from the VA, the Sentinel System, and over 100,000 patient records. They found that clinicians were already following the guidelines 92% of the time. The program wasn’t improving safety-it was blocking access. The decision was based on evidence, not politics.
Will clozapine become easier to get now?
Yes. Experts predict a 25-30% increase in new clozapine starts over the next two years. The biggest barrier wasn’t cost or side effects-it was paperwork. Now that the REMS is gone, more patients will be able to access the most effective treatment for treatment-resistant schizophrenia. Clinics in rural areas and safety-net hospitals expect to start more patients than ever before.


10 Comments
This is huge. I’ve been watching clozapine’s bureaucratic nightmare for years-patients slipping through cracks, clinics collapsing under paperwork, and doctors feeling like accountants instead of healers. The FDA finally got it: safety isn’t about forms, it’s about trust. We’ve known the risks since the 90s. We’ve managed them. Now we can finally treat people, not paperwork.
thank god. my cousin waited 5 weeks last year just because the portal glitched. she almost went back to the hospital. this is life changing
Let’s be real-this isn’t about trust. It’s about cost-cutting. The FDA didn’t remove REMS because doctors were doing great. They removed it because the system was expensive to maintain. Now they’ll shift liability onto clinicians and patients. Watch the neutropenia rates spike in 18 months.
Actually, the data says otherwise. The VA and Sentinel System tracked over 100k patients for a decade. Neutropenia rates stayed flat even as REMS compliance dropped. The system was never preventing harm-it was just making access harder. This change is evidence-based, not political. Good job, FDA.
Typical FDA knee-jerk deregulation. You remove a monitoring system that’s been in place for a decade and suddenly you think everyone’s going to magically follow guidelines? Tell that to the 30% of patients who missed appointments because of transportation issues. This isn’t empowerment-it’s negligence dressed up as progress.
While I appreciate the sentiment, one must acknowledge that the removal of REMS represents a profound epistemological shift in regulatory philosophy-one predicated on the assumption that professional autonomy, when informed by decades of clinical precedent, supersedes institutionalized surveillance. The notion that human judgment, calibrated by longitudinal data and peer-reviewed protocols, can reliably replace algorithmic verification is not merely pragmatic-it is a quiet revolution in medical governance. One wonders whether similar logic might soon be applied to anticoagulants, antiepileptics, or even insulin regimens. The precedent is seismic.
They took away the chains but forgot to hand us the compass. Now we’re free to navigate-but who’s keeping the map? The risk is still there. The silence is louder than the forms ever were.
For the first time in years, I’m actually hopeful for my patients. One man came in last week-he’d been off clozapine for 14 months because his clinic couldn’t keep up with the portal. He cried when I told him he could start again next Monday. This isn’t policy. This is healing.
Finally! I work in a rural clinic in Punjab. We had one patient on clozapine-she traveled 4 hours for blood work. REMS made her wait weeks just to refill. Now she gets her med same day. This is what real care looks like 🙏
As someone who’s worked in both US and Indian psych systems, this is wild. In India, we’ve never had REMS-but we still monitor ANC religiously. Why? Because we care. Not because a database told us to. This move says: trust the clinician. And honestly? It’s about damn time.
Write a comment