Pyridostigmine Overdose Risk Calculator
Overdose Risk Assessment
Assessment Results
Critical Actions
When a medication meant to help you suddenly becomes a danger, knowing what to look for can be the difference between life and death. pyridostigmine bromide overdose is a rare but serious scenario that demands fast recognition and swift medical action. Below you’ll find a clear breakdown of what the drug does, how an overdose shows up, and the exact steps doctors take to save a patient.
What is Pyridostigmine Bromide?
Pyridostigmine bromide is a reversible acetylcholinesterase inhibitor primarily prescribed for Myasthenia gravis and for prophylaxis against nerve agent exposure in military settings. First approved in the 1950s, the drug increases the amount of acetylcholine available at neuromuscular junctions, helping weak muscles contract more effectively.
How Does It Work?
By binding temporarily to the enzyme acetylcholinesterase, pyridostigmine slows the breakdown of acetylcholine. More acetylcholine means stronger electrical signals for muscle fibers, which improves strength in patients with autoimmune muscle weakness. Because the inhibition is reversible, the effect wears off as the drug is cleared, usually within a few hours.
When Does an Overdose Occur?
An overdose can happen if the prescribed dose is exceeded, if pills are taken accidentally or intentionally, or if someone uses the drug without medical supervision (e.g., for performance enhancement). The toxic threshold varies, but taking more than 500 mg in a short period is generally considered dangerous for adults.
Key Signs and Symptoms of Overdose
Because pyridostigmine boosts cholinergic activity, its toxicity mimics a cholinergic crisis. Watch for the following clusters:
- Muscarinic effects - excessive salivation, lacrimation, sweating, and runny nose (often summarized as "SLUDGE").
- Bronchorrhea - heavy mucus production that can obstruct airways.
- Bronchospasm - tightening of airway muscles, leading to wheezing and shortness of breath.
- Bradycardia - heart rate dropping below 60 beats per minute.
- Diarrhea and abdominal cramps.
- Muscle fasciculations - twitching that may progress to weakness or paralysis.
- Respiratory failure - inability to breathe due to airway obstruction or diaphragmatic fatigue.
These symptoms can appear within 30 minutes of ingestion and may rapidly worsen.
Distinguishing Overdose from Other Cholinergic Toxicities
While pyridostigmine toxicity is a form of cholinergic crisis, it differs from nerve‑agent poisoning (e.g., sarin) because the drug does not cross the blood‑brain barrier. Consequently, central nervous system signs such as seizures or coma are less common. The table below highlights the main differences.
| Feature | Pyridostigmine Overdose | Nerve‑Agent Poisoning |
|---|---|---|
| Onset | 30 min-2 h | Seconds-minutes |
| Central effects | Rare | Common (confusion, seizures) |
| Treatment focus | Atropine, supportive care, possible dialysis | Atropine, pralidoxime, oximes, rapid decontamination |
| Typical dose causing toxicity | >500 mg (adult) | Microgram‑level exposure |
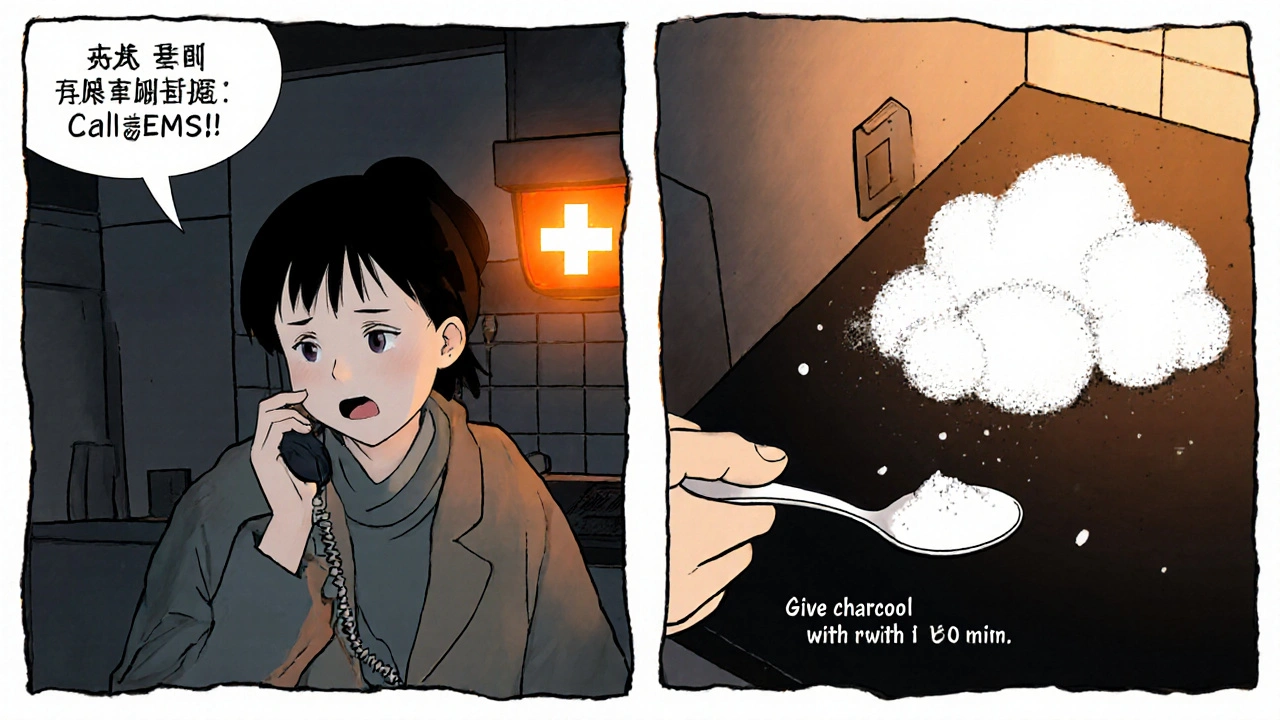
Immediate First‑Aid Steps (What You Can Do Before EMS Arrives)
- Call emergency services and clearly state "possible pyridostigmine bromide overdose."
- If the person is conscious, keep them upright to reduce choking risk.
- Do NOT give anything by mouth unless a medical professional instructs you.
- Administer activated charcoal if it can be obtained within 60 minutes of ingestion - it binds the drug in the GI tract.
- Monitor breathing; if the airway closes, be prepared to perform rescue breaths or CPR.
These actions buy precious time for definitive care.
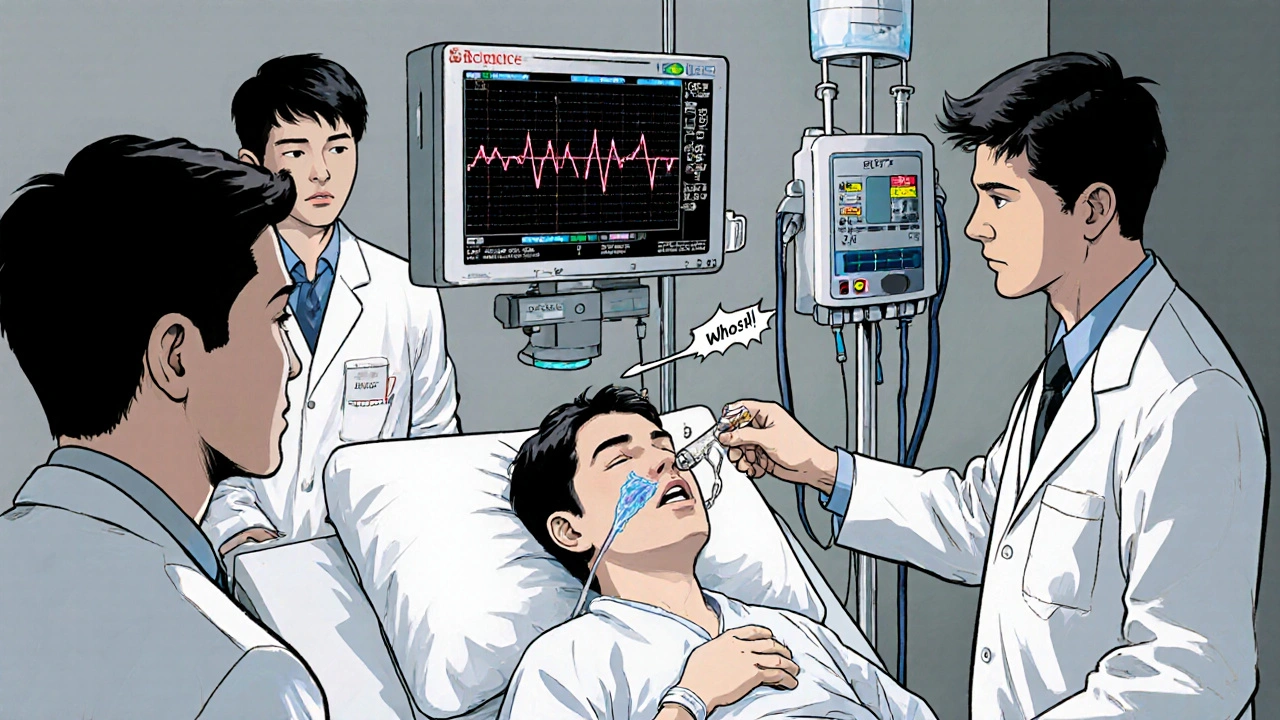
Hospital Management: From ER to ICU
Once the patient reaches the emergency department, the clinical team follows a structured protocol.
- Airway, Breathing, Circulation (ABCs): Intubation is often required because bronchorrhea and bronchospasm can rapidly obstruct the airway.
- Atropine infusion: Administer 0.5-1 mg IV every 5-15 minutes until muscarinic symptoms recede. High‑dose atropine can be life‑saving but watch for tachycardia.
- Pralidoxime (2‑PAM): Although pyridostigmine is reversible, many clinicians give 2‑PAM 30 mg IV bolus then an infusion to protect the neuromuscular junction, especially if mixed with other nerve agents.
- Activated charcoal (repeat): A second dose may be given if the patient presents more than an hour after ingestion and gastric emptying is delayed.
- Hemodialysis or hemoperfusion: In severe cases with very high serum levels, extracorporeal removal can accelerate clearance.
- Supportive care: Electrolyte correction, temperature regulation, and monitoring for secondary infections.
Continuous cardiac telemetry is essential because atropine‑induced tachyarrhythmias may develop.
Prevention: Safe Use and Storage
Preventing an overdose is far easier than treating one. Follow these practical tips:
- Keep the medication in its original container with the label intact.
- Store it out of reach of children and pets - a locked cabinet is best.
- Never share pills, even if the person says they have a similar condition.
- Use a pill organizer that limits the number of doses you can access each day.
- When travelling, carry a copy of the prescription and a brief instruction sheet for emergency personnel.
Regular follow‑up with your neurologist or primary care doctor ensures dosing stays appropriate as your condition changes.
Frequently Asked Questions
Can a mild overdose be treated at home?
Mild excess (e.g., an extra 10 mg) usually causes transient muscle cramps that resolve with dose adjustment. However, any unexpected increase should be reported to a healthcare provider. Home treatment is limited to observation; do not self‑administer antidotes.
Is pyridostigmine bromide safe for pregnant women?
Animal studies show no major teratogenic effects, but human data are limited. Physicians typically weigh the benefits for Myasthenia gravis against potential fetal exposure and may prefer the lowest effective dose.
How long does it take for the drug to leave the system?
Pyridostigmine has a half‑life of about 1-2 hours. Most of the drug is cleared within 6-8 hours, but severe overdose can extend clearance, especially if renal function is impaired.
What distinguishes an atropine reaction from a drug overdose?
Atropine reverses muscarinic symptoms (dry mouth, reduced secretions, faster heart rate). If a patient’s breathing improves after atropine but muscle weakness persists, the underlying pyridostigmine effect is still present, indicating a true overdose.
Can activated charcoal be harmful?
When given to a conscious patient who can protect their airway, charcoal is safe. If the patient is vomiting or has a compromised airway, it may cause aspiration, so medical supervision is critical.
Understanding the warning signs and the exact steps that medical teams follow can save lives. If you or a loved one is prescribed pyridostigmine bromide, keep the information above handy - you never know when quick knowledge could be the difference between a quick recovery and a medical emergency.


9 Comments
The pharmacological profile of pyridostigmine bromide, when examined through the lens of both neuromuscular physiology and toxicology, reveals a delicate balance between therapeutic benefit and the potential for life‑threatening accumulation.
Because the drug exerts its effect by reversibly inhibiting acetylcholinesterase, the resulting elevation of acetylcholine at the neuromuscular junction can swiftly translate into marked muscle strengthening for patients with Myasthenia gravis.
However, this same mechanism underlies the cascade of cholinergic excess that manifests as the classic SLUDGE syndrome when doses exceed the safe threshold.
Clinicians must remain vigilant for the early signs of muscarinic overactivity, such as profuse salivation, lacrimation, and bronchorrhea, which frequently precede more ominous respiratory complications.
The onset of bronchospasm and airway obstruction can progress within minutes, rendering airway protection through timely intubation a critical component of emergency care.
Equally important is the recognition of bradycardia, a manifestation of excessive vagal tone that may demand atropine administration in carefully titrated doses.
From a pharmacokinetic perspective, the relatively short half‑life of one to two hours does not preclude prolonged toxicity in cases of massive ingestion or impaired renal clearance.
Therefore, repeated doses of activated charcoal, when feasible, serve to limit further systemic absorption and expedite gastrointestinal decontamination.
In parallel, the strategic use of atropine infusion, escalating in 0.5‑1 mg increments every five to fifteen minutes, directly counteracts muscarinic symptoms while allowing clinicians to monitor for tachyarrhythmic side effects.
Although pyridostigmine is reversible, many emergency physicians opt to administer pralidoxime (2‑PAM) as an adjunct, particularly when co‑exposure to nerve agents cannot be ruled out.
The rationale for this practice lies in the drug’s ability to reactivate cholinergic receptors that may have become desensitized during the crisis.
In severe scenarios, extracorporeal removal techniques such as hemodialysis or hemoperfusion can be indispensable, especially when serum concentrations remain elevated beyond the expected clearance window.
Continuous cardiac telemetry, alongside vigilant electrolyte monitoring, forms the backbone of supportive care, ensuring that secondary complications are identified promptly.
Patient education regarding proper storage, dose verification, and the perils of unsupervised use stands as the most effective preventive strategy, reducing the likelihood of accidental or intentional overdose.
Ultimately, the collaborative effort of pre‑hospital responders, emergency physicians, and specialized intensive‑care teams determines whether a pyridostigmine bromide toxicity episode culminates in recovery or tragic outcome.
Honestly, most people think a “quick fix” pill can’t turn deadly, but this rundown proves otherwise-don’t be lax.
Listen, if you ever find yourself holding a spare bottle of pyridostigmine without the proper instructions, drop it like a hot coal and call EMS right away; waiting is a luxury you can’t afford, and every second you hesitate the airway tightens.
Keep it locked away; kids aren’t immune to curiosity.
What the mainstream medical community conveniently omits is the shadowy network of undisclosed manufacturers that have been stockpiling pyridostigmine bromide under the guise of national defense contracts.
This hidden supply chain, tightly interwoven with covert research labs, allegedly modifies the compound to enhance its neurotoxic potency, a fact that never sees the light of peer‑reviewed journals.
Consequently, the dosage thresholds quoted in textbooks may be deliberately down‑scaled to mask a more insidious reality where even sub‑therapeutic amounts can accumulate over time in unsuspecting patients.
Moreover, the alleged collaboration between certain pharmaceutical conglomerates and intelligence agencies creates a feedback loop where data on overdose incidents is suppressed, preventing epidemiological awareness.
Such suppression fuels a narrative that pyridostigmine is merely a benign cholinergic enhancer, while in truth it can be weaponized when paired with other organophosphates.
Whispers in the underground forums suggest that ‘dual‑use’ formulations have been dispatched to select units, blurring the line between therapeutic prophylaxis and chemical warfare.
Under these circumstances, standard emergency protocols-relying on atropine and 2‑PAM-may be insufficient, as the altered pharmacodynamics demand higher, risk‑laden dosages.
While governments deny any malfeasance, the pattern of unexplained respiratory failures in civilian populations near military depots raises unsettling questions.
In short, the overt medical literature offers only a sanitized veneer; digging deeper reveals a labyrinth of concealed motives and engineered toxicity.
That extra layer of secrecy makes it even more crucial for us to stay informed and act swiftly when symptoms appear.
If you ever suspect an overdose, do not gamble on home remedies-activate the emergency cascade: call 911, mention pyridostigmine, and keep the person upright if they’re conscious.
Meanwhile, if you have access to activated charcoal, administer it within the first hour; it can dramatically cut absorption.
At the same time, monitor heart rate and breathing closely; a sudden dip in pulse or labored breaths is a red flag that needs immediate medical attention.
Remember, the best defense is proper storage and clear labeling, so accidental ingestion stays out of the picture.
We chase the relief of muscles yet ignore the storm we brew within the synapse a paradox we accept blindly because the world demands performance over caution we must pause and reflect on the hidden cost of convenience
From a pharmacodynamic standpoint, the cholinergic surge induced by pyridostigmine bromide precipitates a muscarinic-dominant response cascade, manifesting as SLUDGE, while the nicotinic component primarily drives fasciculations; therefore, therapeutic modulation requires a bifurcated approach: atropine for muscarinic blockade and, if available, a nicotinic antagonist to attenuate peripheral neuromuscular hyperexcitability.
Whoa, this is intense! 🌟 Remember, knowledge is power-keep that pill bottle out of reach, double‑check every dose, and if anything feels off, scream for help before things go sideways. Together we can dodge the danger and stay strong!
Write a comment