When your lungs can’t expand fully, even simple tasks like walking to the mailbox or tying your shoes become exhausting. That’s often the first sign of pleural effusion-a buildup of fluid between the layers of tissue surrounding your lungs. It’s not a disease itself, but a symptom of something deeper. And if left unaddressed, it can turn serious fast.
What Causes Pleural Effusion?
Pleural effusion happens when fluid leaks into the space between the lung and chest wall. This space is normally filled with just a tiny bit of lubricating fluid. Too much, and your lungs get squeezed. There are two main types: transudative and exudative-and knowing the difference is critical. Transudative effusions come from pressure imbalances in your body. Think of it like water seeping through a weak dam. The most common cause? Congestive heart failure. About half of all transudative cases are tied to it. Other culprits include liver cirrhosis, where your liver stops making enough protein, and nephrotic syndrome, where your kidneys leak protein into your urine. These conditions don’t inflame the pleura-they just change how fluid moves in your body. Exudative effusions are more aggressive. They happen when inflammation, infection, or cancer damages the tiny blood vessels in the pleura, letting fluid, proteins, and cells leak out. Pneumonia is the top cause here, responsible for 40-50% of cases. Cancer comes in second, accounting for 25-30%, especially lung, breast, and lymphoma. Pulmonary embolism, tuberculosis, and autoimmune diseases like rheumatoid arthritis also trigger this type. The key? Not all fluid is the same. In 1972, Dr. Richard Light developed criteria still used today to tell them apart. If your pleural fluid has a protein-to-blood protein ratio over 0.5, an LDH ratio over 0.6, or LDH levels higher than two-thirds of the normal blood value, it’s exudative. These numbers aren’t just academic-they guide what happens next.When and How Is Thoracentesis Done?
If you’re short of breath and imaging shows fluid larger than 10mm on ultrasound, thoracentesis is usually the next step. This is a simple procedure: a thin needle or catheter is inserted between your ribs to drain the fluid. It’s done under ultrasound guidance-no exceptions anymore. Studies show this cuts complications by nearly 80%. The needle typically goes in at the 5th to 7th rib space along the mid-axillary line. For diagnosis, they take 50-100 mL. For relief, they can remove up to 1,500 mL in one go. But there’s a catch: removing too much too fast can cause re-expansion pulmonary edema-a rare but dangerous condition where the lung swells as it re-inflates. The fluid gets tested for protein, LDH, glucose, pH, cell count, and cytology. A pH below 7.20 means the fluid is acidic-often from a complicated pneumonia. Glucose under 60 mg/dL suggests infection or rheumatoid disease. LDH over 1,000 IU/L is a red flag for cancer. Cytology finds cancer cells in about 60% of malignant cases, but sometimes you need multiple samples. Complications happen in 10-30% of cases without ultrasound. Pneumothorax (a collapsed lung) is the most common. Hemorrhage and re-expansion edema are rarer but serious. That’s why doctors now wait until the fluid is clearly visible on ultrasound before proceeding. If you’re stable and the fluid is small, sometimes it’s better to wait and monitor.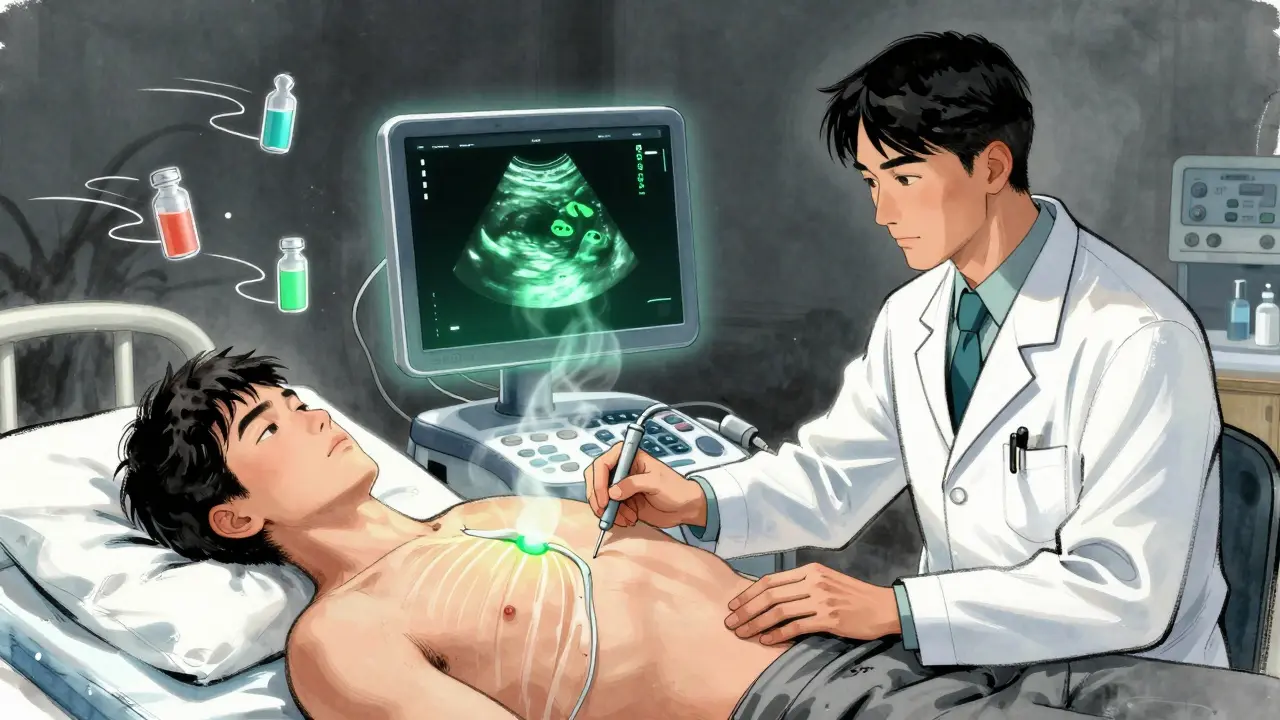
How to Stop Pleural Effusion from Coming Back
Draining the fluid gives you relief-but it doesn’t fix the problem. Without treating the root cause, it will return. That’s why recurrence prevention starts with diagnosis. For heart failure-related effusions, the fix is medical: diuretics, ACE inhibitors, beta-blockers, and monitoring NT-pro-BNP levels. When treatment is guided by these biomarkers, recurrence drops from 40% to under 15% in three months. No surgery needed. Just better management of the heart. Malignant effusions are trickier. After a single thoracentesis, half of them come back within 30 days. That’s why doctors don’t stop at drainage. For patients with a good life expectancy, talc pleurodesis is the gold standard. It involves injecting sterile talc into the pleural space to glue the lung to the chest wall. Success rates? 70-90%. But it’s painful-60-80% of patients need strong pain control. A better option for many? Indwelling pleural catheters. These are tiny tubes left in place for weeks. You or a caregiver can drain fluid at home, often just a few ounces at a time. Studies show 85-90% of patients avoid hospital readmissions after six months. And unlike pleurodesis, you can still treat the cancer without being stuck in the hospital. One trial showed hospital stays dropped from over a week to just two days. For parapneumonic effusions (those from pneumonia), antibiotics alone aren’t enough if the fluid is thick or infected. If the pH is below 7.2, glucose under 40 mg/dL, or the fluid tests positive for bacteria, you need drainage. Left untreated, 30-40% of these turn into empyema-pus in the chest. That requires surgery. Even after heart surgery, fluid can collect. About 15-20% of patients get it. Most resolve on their own, but if more than 500 mL drains per day for three days straight, doctors will leave a chest tube in longer. With proper management, recurrence drops to 5%.
What Doesn’t Work-and Why
Not every fluid collection needs a needle. A 2019 JAMA study found that 30% of thoracenteses were done on small, asymptomatic effusions-and didn’t change anything. You didn’t feel better. You didn’t get a diagnosis. You just got poked. Also, chemical pleurodesis isn’t recommended for non-cancer effusions. There’s no proof it helps. It just adds pain and risk. The American Thoracic Society says: don’t do it unless it’s cancer or a trapped lung. And don’t ignore the basics. If you have heart failure, don’t skip your meds. If you’re a smoker with lung cancer, quitting improves outcomes. If you’ve had pneumonia, finish your antibiotics. Recurrence isn’t bad luck-it’s often missed management.The Big Picture: Treat the Cause, Not Just the Fluid
Dr. Light, who gave us the criteria still used today, put it best: “Treating the effusion without treating the cause is like bailing water from a sinking boat without patching the hole.” Today’s approach is smarter. We don’t just drain. We test. We analyze. We personalize. Ultrasound isn’t a luxury-it’s standard. Indwelling catheters aren’t experimental-they’re first-line for many cancer patients. Biomarkers guide therapy. And survival? For malignant effusions, five-year survival has doubled since 2010 because we’re treating the cancer better, not just the fluid. If you’ve been diagnosed with pleural effusion, ask: What’s causing this? Is it heart failure? Cancer? Infection? Once you know, the path forward becomes clear. Drainage helps. But real relief comes from fixing what’s underneath.What are the most common causes of pleural effusion?
The most common cause of transudative pleural effusion is congestive heart failure, accounting for about half of all cases. For exudative effusions, pneumonia is the top cause, followed by cancer-especially lung, breast, and lymphoma. Pulmonary embolism, tuberculosis, and autoimmune diseases like rheumatoid arthritis are also frequent contributors.
Is thoracentesis safe?
Yes, when done with ultrasound guidance, thoracentesis is very safe. Complications like pneumothorax (collapsed lung) drop from nearly 19% to under 5% when ultrasound is used. Other risks include bleeding and re-expansion pulmonary edema, but these are rare. Most patients tolerate the procedure well with local anesthesia.
How do doctors tell if pleural fluid is from cancer?
Cytology-examining the fluid under a microscope for cancer cells-is the main test. It finds cancer in about 60% of cases. If cytology is negative but suspicion remains, doctors may repeat the test, order a pleural biopsy, or use biomarkers like LDH over 1,000 IU/L or low glucose levels as clues. Imaging and patient history also help confirm the diagnosis.
Can pleural effusion come back after treatment?
Yes, especially if the underlying cause isn’t treated. After a simple drainage, malignant effusions return in about 50% of cases within 30 days. Heart failure-related effusions can recur if diuretics aren’t properly managed. But with targeted treatments-like indwelling catheters for cancer or optimized heart meds for CHF-recurrence rates can drop to 15% or lower.
What’s the difference between pleurodesis and an indwelling pleural catheter?
Pleurodesis uses chemicals like talc to scar the pleural layers together, permanently sealing the space. It’s effective (70-90% success) but often painful and requires hospitalization. An indwelling pleural catheter is a small tube left in place for weeks. You drain fluid at home as needed. Success rates are similar (85-90%), but it’s less invasive, avoids hospital stays, and allows continued cancer treatment. It’s now preferred for many patients with recurrent malignant effusions.
Do I need to be hospitalized for pleural effusion treatment?
Not always. Simple diagnostic thoracentesis can be done in an outpatient clinic. For malignant effusions, indwelling catheters are often inserted as outpatient procedures. Hospital stays are usually only needed for complicated cases-like empyema, large effusions requiring drainage, or if you’re too sick to manage at home. Many patients with cancer can now manage fluid at home with a catheter, avoiding repeated hospital visits.

10 Comments
This made me cry. I lost my dad to this. They drained him three times and he still couldn’t breathe right. No one ever told us it was just bandaids on a bullet wound.
Now I scream at every doctor who says 'it's just fluid.' It's not just fluid. It's his body screaming for help and nobody listens.
In India, we see this often with TB and heart failure. Many patients come too late because they think it's just a cough or fatigue from work. The real problem is access-ultrasound machines are rare in rural clinics. We need more training, not just more procedures.
Light’s criteria still work here. But without labs, even that is a luxury.
Look, I’ve seen this a hundred times in the ER. People think thoracentesis is a cure. It’s not. It’s a diagnostic tool. I had a guy last month who got drained twice, then came back with a collapsed lung because he ignored his CHF meds.
Stop chasing the fluid. Start chasing the cause. Diuretics aren’t optional. They’re your lifeline. And if you’re a smoker with cancer? Quit. Not tomorrow. Today.
bro i had this last year 😭 they stuck a needle in my side and i thought i was gonna die
then they said 'oh its probably cancer' and i was like ok cool guess i'm dying
turns out it was just pneumonia but still… why do they make it sound like a horror movie?
also i still have the catheter lol its like a secret water spout in my chest 🤫💧
why do doctors always make this so complicated
just drain it and be done with it
why do you need all these ratios and labs and catheters
its just water in the chest
why not just poke it and move on
they just wanna bill you more
my cousin got drained once and lived for 5 years
so who cares about all this science stuff
just fix it
I appreciate how this breaks down the science without losing the humanity. I work with elderly patients who often don’t understand why they can’t just 'get the fluid out' and feel better.
It’s hard to explain that the body isn’t a leaky bucket. It’s a system. And treating the system takes patience.
Thank you for writing this with clarity and care.
Okay but have you heard about the 2021 CDC memo that says 63% of pleural effusions are misdiagnosed because hospitals are using outdated ultrasound protocols?
And why is talc still being used when it’s been linked to asbestos contamination in 12% of batches? Nobody talks about this.
Also-why do they never mention that heart failure patients on diuretics often develop kidney damage from over-draining? It’s all just profit-driven band-aid medicine.
They’re not treating you. They’re managing liability.
Let’s be real-this whole system is a performance. The Light criteria? A 50-year-old mathematical hack that still governs life-or-death decisions.
The indwelling catheter? A corporate invention designed to shift care from hospitals to homes so insurers save money-not because it’s better for patients.
And don’t get me started on cytology. Sixty percent accuracy? That’s gambling. We’re playing Russian roulette with biopsy results while patients gasp for air.
We don’t need more tests. We need a new paradigm. One that doesn’t treat the body like a broken machine to be fixed with needles and numbers.
This isn’t medicine. It’s triage capitalism.
I’ve been researching this since my mom’s diagnosis. The way this post explains transudative vs exudative is actually the first time I felt like I *got* it.
It’s like comparing a flooded basement from a broken pipe (heart failure) versus a burst water main caused by an earthquake (cancer or infection).
One you fix the pipe. The other? You need to rebuild the whole city.
And the catheter thing? Mind blown. I never realized you could drain at home like a coffee machine. That’s beautiful.
Also-LDH over 1000? That’s not a number. That’s a scream.
Just wanted to add something practical: if you or a loved one has a pleural catheter, keep a log. Write down how much you drain, when, and how you feel afterward.
It sounds simple, but when you show that to your oncologist or pulmonologist, they can adjust the schedule-sometimes even reduce visits.
Also, don’t be afraid to ask for pain meds before draining. It’s not weakness. It’s self-care.
This isn’t just medical info-it’s a toolkit for living better with chronic illness.
Write a comment