What Parkinson’s Disease Really Feels Like
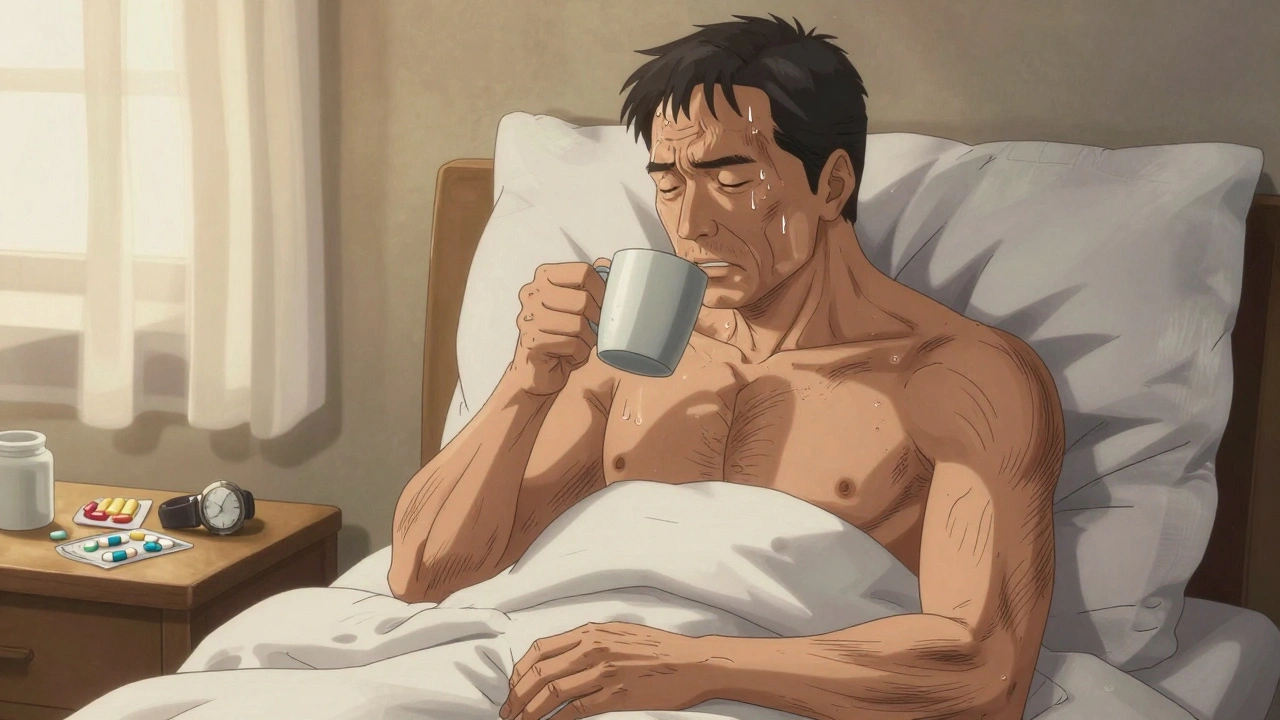
Imagine waking up and your hand won’t stop trembling, even when you’re trying to hold a coffee cup. Your movements feel heavy, like walking through thick mud. Buttoning a shirt takes twice as long. You forget to swallow, and saliva pools in your mouth. This isn’t just aging-it’s Parkinson’s disease. It’s not one symptom. It’s a cascade of changes that quietly steal your independence, one small motion at a time.
As of 2023, about 1 million people in the U.S. are living with Parkinson’s. Most are over 60, but 1 in 25 are diagnosed before 50. The disease doesn’t just shake your hand-it reshapes your life.
The Four Core Motor Symptoms
Doctors don’t diagnose Parkinson’s with a blood test or scan. They watch how you move. There are four key signs, and you need at least two to be considered for diagnosis. But here’s the catch: not everyone has all of them.
- Tremor is what most people picture: a rhythmic shaking, often starting in one hand. It’s called a "pill-rolling" tremor because it looks like you’re rolling a pill between your thumb and finger. It happens when you’re resting. If you pick up the cup, it stops. About 70% of people first notice this symptom.
- Rigidity means your muscles stay tight, even when you’re trying to relax. It can feel like bending a stiff pipe. Some people have "cogwheel" rigidity-where the resistance comes in little jerks, like a gear turning. Others have "lead-pipe" rigidity-a constant, smooth stiffness. About 85% experience the cogwheel type.
- Bradykinesia is the most important symptom. It means slowness of movement. Not just slow walking. Slow blinking. Slow speech. Slow to get out of a chair. Your face may lose expression, called hypomimia. You blink less. Your handwriting shrinks into tiny, cramped letters-micrographia. This symptom is present in nearly every patient, often before tremor shows up.
- Postural instability is the late-stage trouble with balance. You lean forward. You take small, shuffling steps. You don’t swing your arms when you walk. This increases fall risk dramatically. Most people don’t have this until 5 to 10 years after diagnosis.
Bradykinesia is the silent anchor of Parkinson’s. Without it, you don’t have Parkinson’s. Even if your tremor disappears, if your movements are slow and stiff, the diagnosis holds.
Other Motor Signs You Might Not Notice
There’s more than the big four. These symptoms fly under the radar but can be just as disabling.
- Dystonia causes painful muscle spasms. In younger patients, it often starts in the foot, twisting it inward. It can happen at night or when medication wears off.
- Stooped posture affects 65-80% of people. You don’t just hunch-you lose your natural spinal curve. It’s not just bad posture. It’s your body adapting to stiffness and imbalance.
- Reduced arm swing happens early. One arm stops moving when you walk. Then both do. This isn’t just awkward-it throws off your balance. About 75% of people lose this natural rhythm.
- Speech changes are common. Your voice gets softer-5 to 10 decibels quieter. That’s like speaking from across the room instead of beside someone. 89% develop a quiet voice. 74% get slurred speech.
- Drooling and swallowing trouble happen because you stop swallowing as often. Saliva builds up. You might not even notice you’re drooling until someone points it out. Swallowing problems affect 35-80% of people, depending on how far the disease has progressed. This is dangerous-it raises the risk of choking or pneumonia, which causes 70% of Parkinson’s-related deaths.

How Medications Work-and Where They Fall Short
There’s no cure. But there are drugs that help. They don’t stop the disease. They replace what your brain has lost: dopamine.
Levodopa is the gold standard. It’s been around since 1967. Your body turns it into dopamine. For most people, it works wonders-at first. About 70-80% of patients see big improvements in movement. But after 5 years, about half develop problems: motor fluctuations (medication wearing off between doses) and dyskinesias (involuntary, dance-like movements).
Dopamine agonists like pramipexole and ropinirole mimic dopamine without turning into it. They’re often used first in younger patients to delay levodopa side effects. They help about half of early-stage patients. But they come with their own risks: sleep attacks, impulse control problems, and swelling in the legs.
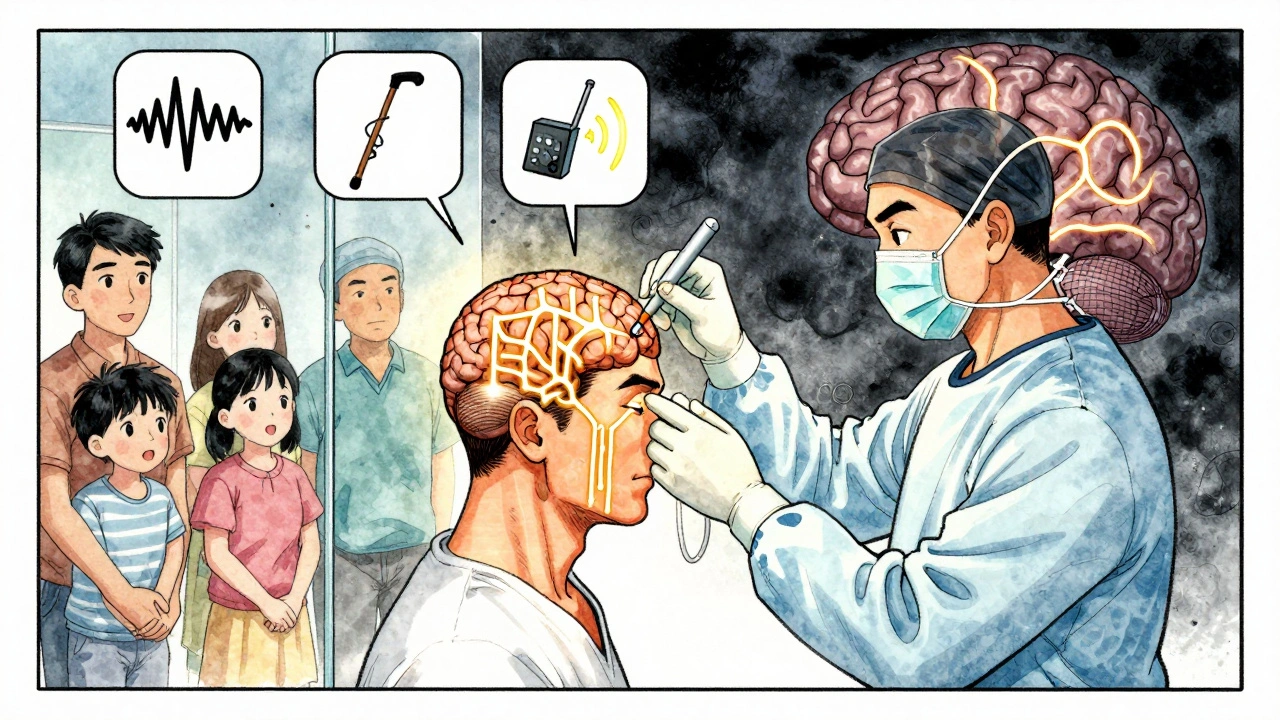
For people who’ve been on levodopa for 10+ years and still struggle, deep brain stimulation (DBS) becomes an option. About 30% of patients eventually get it. A surgeon implants electrodes in your brain. A pacemaker-like device sends pulses to block the faulty signals. It doesn’t cure Parkinson’s. But it can cut tremors, reduce dyskinesias, and give you back 2-4 hours of good movement each day.
There are no drugs that slow the disease. Not yet. Research is looking at alpha-synuclein- a protein that clumps in Parkinson’s brains-but nothing has proven to stop progression in large trials.
Daily Life: The Hidden Struggles
Medications help you move. But they don’t fix the little things that make life hard.
- Getting out of bed takes effort. Turning over feels impossible. About 65% of people report this within 5 years.
- Dressing becomes a chore. Buttoning a shirt? It takes 3.1 times longer than it used to. Putting on socks? You might need a long-handled tool.
- Walking changes. Your steps get shorter-25-35% shorter. Your speed drops by 30-40%. You shuffle. You don’t lift your feet. This is why 68% of people fall at least once a year. 30% fall repeatedly.
- Communication gets harder. People ask you to repeat yourself. You stop joining conversations because it’s exhausting. Your voice fades. You feel isolated.
- Sexual function drops in 50-80% of men. It’s not just about desire. It’s about movement, sensation, and medication side effects. Most doctors never ask. Most patients never bring it up.
- Akathisia is a restless urge to move. You can’t sit still. You pace. You shift constantly. It’s not anxiety-it’s a side effect of dopamine therapy. It affects 15-25% of people.
These aren’t "inconveniences." They’re barriers to dignity. They make you feel like a burden. They erode your sense of self.
What Actually Helps Beyond Pills
Medication isn’t the whole story. Movement is medicine.
Physical therapy isn’t optional-it’s essential. A 12-week program focused on balance, strength, and gait can improve walking speed by 15-20% and cut fall risk by 30%. Tai chi, boxing, dancing-these aren’t hobbies. They’re therapy. They retrain your brain to move.
Speech therapy helps with voice volume and swallowing. You learn techniques to project your voice. You practice swallowing safely. It’s not glamorous, but it keeps you out of the hospital.
Occupational therapy teaches you how to adapt. Grabbers for clothes. Non-slip mats. Raised toilet seats. Voice amplifiers. These tools don’t fix Parkinson’s. But they let you keep doing things on your own.
And nutrition matters. Swallowing problems mean you might not get enough calories or protein. A dietitian can help you choose softer, nutrient-dense foods. You need to avoid choking risks-but you also need to stay strong.
Where Things Stand Today
Parkinson’s doesn’t have a cure. But it’s not a death sentence. People live for decades with it. The key is early recognition and proactive management.
If you notice a tremor that won’t go away, or your movements feel slower, or you’re falling more often, don’t wait. See a neurologist who specializes in movement disorders. The sooner you start treatment, the better you can control symptoms.
It’s not about fighting the disease. It’s about staying in control of your life. Medications help. Therapy helps. Support helps. You don’t have to do it alone.
Frequently Asked Questions
Can Parkinson’s be diagnosed with a scan?
No. There’s no blood test or MRI that confirms Parkinson’s. Doctors diagnose it by observing motor symptoms-especially bradykinesia-along with tremor or rigidity. A dopamine transporter scan (DaTscan) can help rule out other conditions, but it can’t confirm Parkinson’s on its own. Diagnosis is clinical, based on movement.
Why does levodopa stop working over time?
Levodopa doesn’t stop working-it’s your brain’s ability to process it that changes. As Parkinson’s progresses, dopamine-producing cells keep dying. The brain loses its ability to store and release dopamine steadily. This leads to "on-off" fluctuations: you feel great right after a dose, then suddenly stiff and slow. High doses can also trigger dyskinesias-uncontrolled movements. Adjusting timing, adding other drugs, or switching to DBS can help.
Is Parkinson’s hereditary?
Most cases aren’t inherited. Only about 10-15% have a clear genetic link. Even then, having a gene mutation doesn’t guarantee you’ll get Parkinson’s. Age, environment, and other unknown factors play bigger roles. If you have a parent with Parkinson’s, your risk is slightly higher-but still low overall.
Can exercise really make a difference?
Yes-and not just for mobility. Studies show regular exercise improves balance, reduces falls, boosts mood, and may even protect brain cells. People who walk 2.5 hours a week or do strength training twice a week report better quality of life. You don’t need to be an athlete. Dancing, swimming, tai chi, or even vigorous gardening counts. Movement signals the brain to stay active.
What should I do if I start falling more often?
Falls are a red flag. Don’t ignore them. Talk to your doctor and ask for a physical therapy evaluation. They’ll check your balance, strength, and gait. You may need a cane or walker. Remove rugs and clutter at home. Install grab bars in the bathroom. Consider a medical alert system. Most falls happen in the home. Prevention is simple-but only if you act early.
Are there foods I should avoid?
Avoid high-protein meals right before or after taking levodopa. Protein competes with levodopa for absorption in the gut. Take your medication 30-60 minutes before meals. Also, avoid excessive alcohol and sugary drinks-they can worsen balance and cause dehydration. Eat fiber-rich foods to prevent constipation, which is common in Parkinson’s.
What Comes Next
If you’re newly diagnosed, start with a neurologist who specializes in movement disorders. Don’t settle for a general neurologist if you can avoid it. Find a Parkinson’s clinic if one’s nearby.
Join a support group. Talk to others who get it. You’ll learn more from them than from any brochure.
Start moving-today. Even if it’s just walking around the block. Your brain needs it.
Parkinson’s changes your body. But it doesn’t have to change who you are. You still have control. You still have voice. You still have choices. The goal isn’t to beat the disease. It’s to live well with it-every single day.

15 Comments
Remarkably thorough exposition on the clinical and lived dimensions of Parkinson’s disease. The delineation between motor symptoms and their functional ramifications is both precise and humane. One cannot help but appreciate the emphasis on bradykinesia as the cardinal sign-too often overshadowed by tremor in popular discourse. This is precisely the kind of content that elevates public understanding beyond sensationalism.
It’s not the disease, it’s the *narrative*.
I’ve seen this up close with my dad. The way he’d sit there, smiling, but his hands just… wouldn’t still. It broke my heart. But we started doing tai chi together twice a week. He still moves slower, but he laughs louder now. And that’s something. Keep moving, even if it’s small. It counts.
My mom had Parkinson’s for 12 years. The biggest thing nobody talks about? The shame. Drooling in public, forgetting how to button your shirt, needing help to pee. It’s not the tremors. It’s feeling like a ghost in your own body. But therapy helped. Speech therapy saved her from pneumonia. PT kept her from falling. And yeah, dancing with her in the kitchen once a week? That was medicine too. Don’t underestimate joy.
For anyone reading this and thinking about DBS-talk to a movement disorder specialist before you decide. It’s not a cure, but for many, it’s the difference between being trapped and being present. My brother got it after 15 years on levodopa. The dyskinesias were brutal. After surgery? He could hold his coffee again. Not perfectly. But enough. And that’s huge.
HAHAHAHA! You people in America think you’re so advanced with your fancy brain implants and your $100,000 therapies-yet in India, we’ve had yoga, ayurveda, and spiritual discipline for 5,000 years! You’re treating symptoms like children with toys, while we’ve always known the soul is the cure! Why do you ignore the wisdom of the East? This is cultural arrogance disguised as science!
bradykinesia? more like brady-why-did-i-even-bother-to-write-this
Did you know the FDA approved levodopa in 1967 because Big Pharma wanted to control the dopamine narrative? The real cause is glyphosate in your food and 5G signals messing with your basal ganglia. They don’t want you to know that natural magnesium and grounding can reverse this. Watch the documentary ‘Parkinson’s: The Cover-Up’-it’s on YouTube. They’re silencing the truth.
Oh wow, another article telling people to "just exercise more" like it’s that easy. You think someone who can’t lift their foot off the floor is going to join a boxing class? Maybe if you weren’t so busy patting yourself on the back for being "aware," you’d actually listen to patients instead of writing feel-good lists.
It’s wild how Parkinson’s turns the body into a broken symphony-tremors as dissonant notes, rigidity as a stuck string, bradykinesia as a metronome that forgot the tempo. And yet… people still dance. Still laugh. Still sip coffee with shaking hands. There’s something profoundly beautiful in that stubbornness. The brain may decay, but the spirit? It learns new languages.
WAIT-so you’re telling me this isn’t just a government mind-control experiment to make old people slow down so they don’t vote? I’ve been noticing how everyone walks like zombies lately. And the drooling? That’s the chip leaking fluid! They’re turning us into docile drones with dopamine manipulation! I saw a man at Walmart today-he had a tiny blinking light on his collar. I KNOW IT.
my grandpa had parkinsons and he used to just sit there like a statue and i thought he was mad at me. turns out he just couldn’t move. i feel so bad now. also i hate when people say "you’re so strong" like it’s a compliment. it’s not. it’s just sad.
To the person who said "it’s not the disease, it’s the narrative"-you’re not wrong. But the narrative matters because it shapes care. This post? It doesn’t just inform-it validates. For every person reading this who feels invisible, this is a mirror. And for every caregiver who thinks they’re doing enough? This is a roadmap. This isn’t just information. It’s a lifeline.
The statistical precision of this article is commendable. The inclusion of prevalence rates, symptom progression timelines, and pharmacokinetic limitations demonstrates a rigorous adherence to evidence-based reporting. A notable departure from the often emotionally manipulative tone of disease narratives. Well done.
There’s a quiet metaphysics here, isn’t there? The body, once a vessel of effortless motion, becomes a cathedral of resistance. Each tremor, each frozen step-a silent hymn to impermanence. We chase dopamine like a god, but perhaps the real miracle isn’t in replacing it… but in learning to live with its absence. To move, not because we can, but because we choose to. Even when the world forgets to listen.
Write a comment