Every year, more than 2,000 workers in the U.S. die from lung diseases caused by breathing in dust and fibers they were exposed to on the job. These aren’t random accidents. They’re preventable. Yet, they keep happening - in construction sites, mines, factories, and demolition crews. Two of the most common and deadly are silicosis and asbestosis. Both are irreversible. Both are silent until it’s too late. And both can be stopped - if the right steps are taken.
What Is Silicosis, and How Does It Happen?
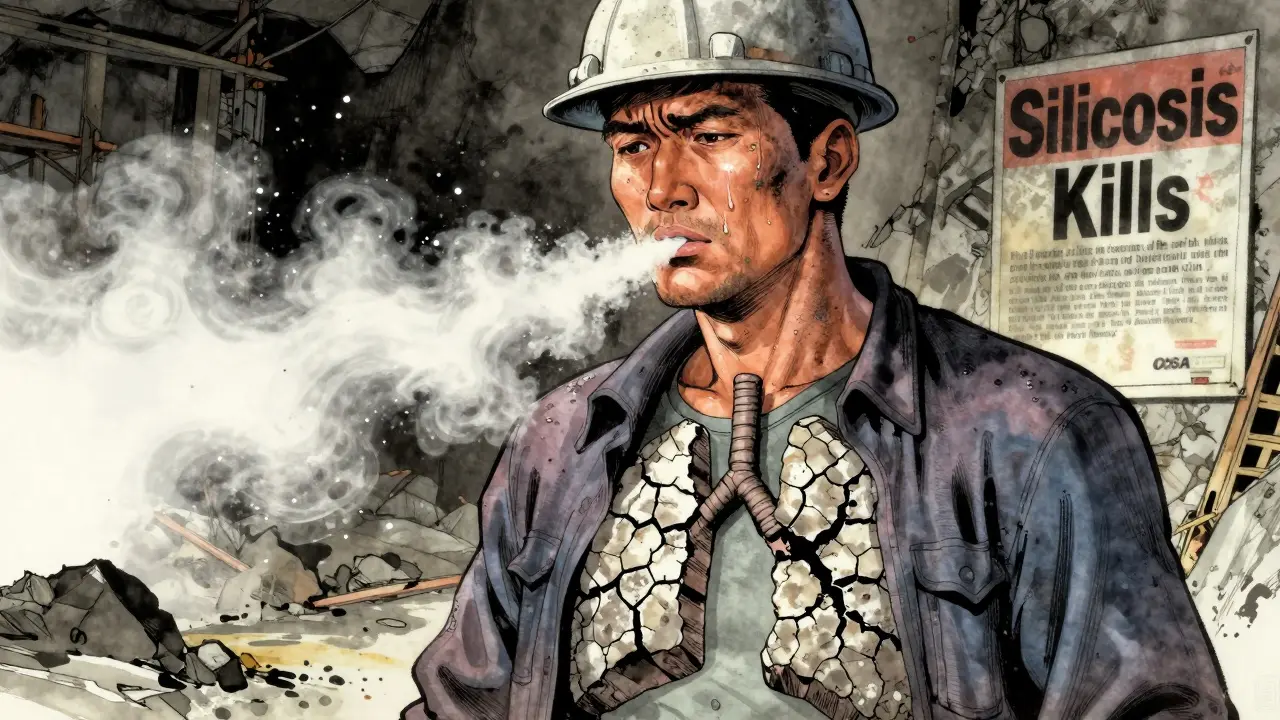
Silicosis is caused by breathing in crystalline silica dust. This isn’t just any dust. It’s the same stuff found in sand, stone, concrete, and granite. When workers cut, drill, grind, or blast these materials, tiny particles become airborne. Once inhaled, these particles cut into lung tissue, triggering inflammation and scarring. Over time, the lungs stiffen. Breathing becomes harder. Coughing, fatigue, and shortness of breath follow.
It doesn’t happen overnight. Most cases develop after 10 or more years of exposure. But in high-risk jobs - like sandblasting or cutting engineered stone countertops - people can develop aggressive forms in just a few years. In 2018, NIOSH estimated silicosis caused around 1,200 deaths annually in the U.S. That number hasn’t dropped.
What’s worse? Silicosis doesn’t just kill. It increases the risk of tuberculosis, lung cancer, and kidney disease. And once the scarring sets in, there’s no cure.
What Is Asbestosis, and Why Is It Still a Problem?
Asbestosis comes from asbestos fibers - a mineral once used in insulation, roofing, pipes, and floor tiles. When these materials age or get disturbed, fibers break loose and float in the air. Inhaling them causes scarring deep in the lungs, similar to silicosis. But asbestos fibers are even harder for the body to clear. They stay lodged for decades.
The first confirmed case was in 1906, in a London asbestos factory worker. Today, it’s still killing people. Between 2004 and 2014, 1,163 U.S. workers died from asbestosis, according to CDC data. Many of those deaths came from older buildings being renovated or demolished. The EPA estimates 733,000 public buildings in the U.S. still contain asbestos. That means every renovation, every repair, every demolition is a potential exposure risk.
Like silicosis, asbestosis has no cure. It slowly destroys lung function. And because it takes 20 to 30 years to show symptoms, many workers don’t connect their breathing problems to their job until it’s too late.
The Hierarchy of Control: What Actually Works
Preventing these diseases isn’t about hoping workers wear masks. It’s about removing the hazard at the source. The CDC and OSHA have a clear hierarchy for this:
- Elimination - Don’t use silica or asbestos at all. Replace engineered stone with safer materials. Use non-asbestos insulation.
- Substitution - If you can’t eliminate, swap in safer alternatives. Wet-cutting methods reduce silica dust by 90% compared to dry cutting.
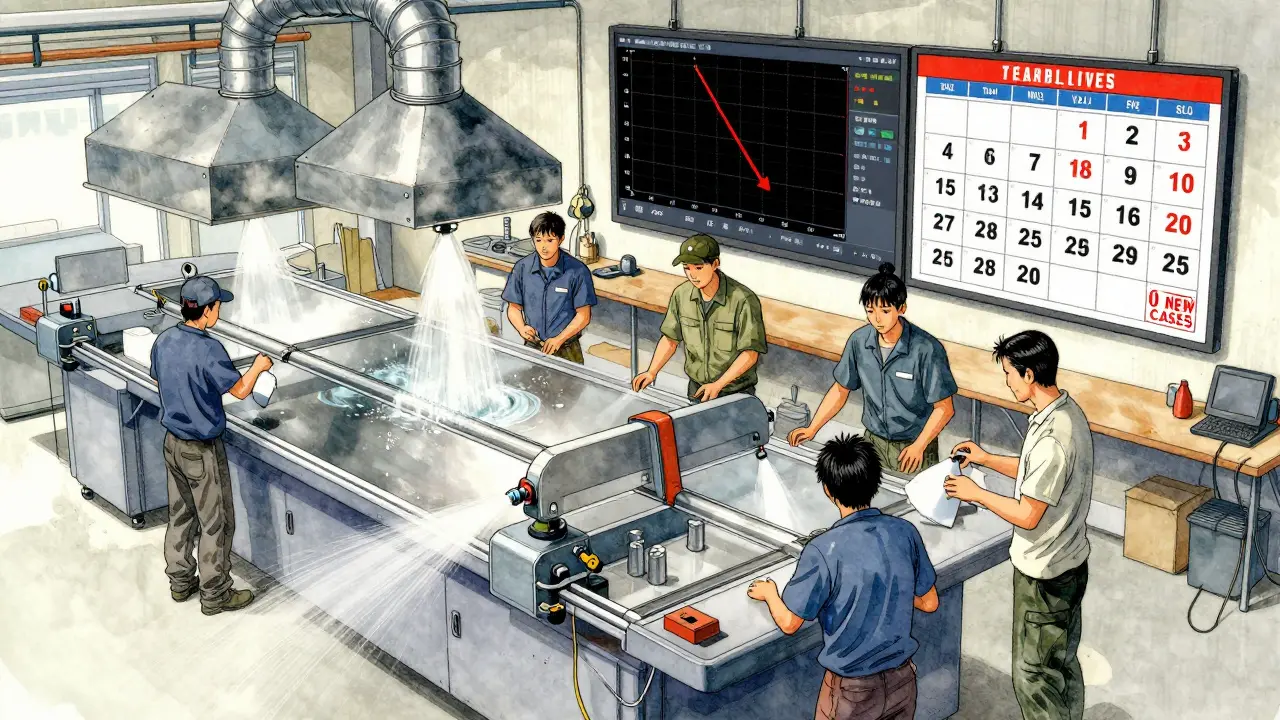
- Engineering Controls - This is where most success happens. Local exhaust ventilation systems that pull dust away at 100-150 feet per minute can cut exposure by 70-90%. Sealing off cutting areas to contain 95% of dust is another proven method.
- Administrative Controls - Limit how long workers are exposed. Rotate tasks. Schedule dusty work for times when fewer people are around.
- PPE - Respirators are the last line of defense. N-95 masks filter 95% of particles 0.3 microns in size. P-100 masks filter 99.97%. But here’s the catch: if they’re not worn correctly, they do nothing.
Engineering controls work best. They protect everyone nearby, not just the person wearing a mask. They’re also more reliable than relying on human behavior.
Why PPE Alone Fails - And What Workers Really Say
OSHA requires fit testing for respirators every year. But a 2022 NIOSH report found that 68% of worker complaints about respiratory protection were about discomfort or poor fit. In 32% of cases, workers modified their masks to breathe easier - which made them useless.
On Reddit’s r/Construction, one worker wrote: “My company got wet saws last year. Dust dropped. But the foreman still yells at us for taking too long with water.” Another said: “I worked demolition for 15 years. Never had a proper fit test until OSHA showed up.”
And it’s not just about fit. In 90-degree heat, wearing a P-100 respirator is exhausting. One industrial hygienist on r/OccupationalMedicine reported compliance drops to 40% in summer. That’s not negligence. That’s a system failure.
PPE is necessary - but only when everything else fails. Relying on it as the main defense is like putting a bandage on a broken leg.

Who’s at Risk? Industries That Still Ignore the Rules
Construction, mining, and manufacturing make up 75% of occupational lung disease cases. But it’s not just the big companies.
Small businesses - those with fewer than 20 employees - are the most vulnerable. Wisconsin Department of Health data from 2021 showed 78% of them had no formal respiratory protection program. That’s not because they’re evil. It’s because they don’t know how to start. Training costs money. Equipment costs money. And many don’t realize how deadly the dust really is.
OSHA fined over 1,000 construction companies for silica violations in 2021 alone. Total fines: $3.2 million. That’s not just a slap on the wrist. It’s a warning. These aren’t rare violations. They’re systemic.
What Prevention Actually Looks Like - Real Examples
Successful prevention isn’t about posters on the wall. It’s about action.
One Oregon-based stone fabrication shop switched from dry cutting to wet cutting. They installed local exhaust hoods on every saw. They trained every employee - not just a one-hour video, but hands-on demos with real dust samples. Within a year, their respiratory complaints dropped by 80%.
A demolition crew in Chicago started using HEPA-filtered vacuums on every grinder. They assigned a safety lead to check respirator fit every morning. They let workers know: “If your mask itches, we’ll find you a better one.” Compliance jumped from 55% to 92%.
Both cases followed the same rule: exposure reduction comes from the job, not the mask.
Health Monitoring: Catching It Before It’s Too Late
Even with perfect controls, mistakes happen. That’s why regular health checks matter.
The American Thoracic Society recommends spirometry testing - a simple breathing test - at baseline and every five years for exposed workers. For those with existing lung issues, it should be annual.
Why? Because lung damage from silicosis and asbestosis shows up on spirometry long before symptoms do. One study found that early detection and removing workers from exposure can slow disease progression by 30-50%.
It’s not about finding who’s sick. It’s about protecting who’s still healthy.
The Bigger Picture: Why This Isn’t Just a Worker Issue
These diseases don’t just hurt workers. They hurt families. They hurt communities. They hurt the economy.
Workers with silicosis or asbestosis often can’t return to work. Many need oxygen tanks. Some need lung transplants. The average workers’ compensation claim for these diseases runs over $150,000 - and that’s just the medical part.
And the cost isn’t just financial. It’s emotional. Imagine knowing your breathing problems came from your job - and that your employer could have stopped it.
The European Respiratory Society says 60-70% of these cases could be prevented with current technology. The American Lung Association says the same. So why are we still seeing new cases in 2025?
Because prevention isn’t about technology. It’s about will.
What Needs to Change - And How You Can Help
Here’s what works:
- Use wet methods for cutting stone or concrete.
- Install local exhaust ventilation on every tool that creates dust.
- Require P-100 respirators with fit testing - no exceptions.
- Train workers for 4-6 hours, not 15 minutes.
- Test lungs annually for anyone exposed to silica or asbestos.
- Hold supervisors accountable. If they don’t wear a mask, they shouldn’t expect others to.
If you’re a worker: speak up. If you’re a supervisor: lead by example. If you’re a business owner: invest in controls. It pays back in 18-24 months through fewer injuries, lower insurance, and less turnover.
The technology exists. The rules are clear. The science is settled. The only thing missing is the commitment.
These diseases don’t have to be part of the job. They never should have been.
Emerging Tools and What’s Next
NIOSH launched the ‘Prevent eTool’ in 2023 - a free digital guide for 15 high-risk industries. Companies using it saw a 40% drop in respiratory incidents in just six months.
Wearable dust sensors are now being tested on construction sites. They give real-time alerts when silica levels spike. Imagine getting a text on your phone: “Dust too high. Stop work.” That’s not science fiction. It’s coming fast.
And the goal? The European Respiratory Society wants to eliminate occupational lung diseases by 2030. It’s ambitious. But with today’s tools, it’s possible.

12 Comments
Had a cousin who worked in stone fabrication for 12 years. Never wore a mask because ‘it felt like suffocating.’ Got diagnosed with silicosis last year. Now he’s on oxygen three hours a day. This post hits hard because it’s not theoretical. It’s real people. The wet-cutting and exhaust systems aren’t luxuries-they’re lifelines. Companies that skip them are gambling with lives.
And honestly? The fact that we still have to argue this in 2025 is criminal.
PPE is a bandaid on a bullet wound and everyone knows it but nobody wants to pay for the real fix
That Chicago demolition crew story gave me chills in the best way.
They didn’t just ‘follow rules’-they treated people like humans. That’s the difference between compliance and culture.
Also if your mask itches you deserve a better one 😊
Let me guess-this is another left-wing scare tactic to shut down construction and make people dependent on government handouts.
Silica? That’s just dirt. Asbestos? Been in buildings since the 1920s. You think we’re going to tear down every school and hospital because some bureaucrat says so?
My grandpa worked on the Hoover Dam with no mask and lived to 92. You think he was ‘exploited’? Nah. He was proud. Now we’ve got a whole industry built on fear and lawsuits.
And don’t even get me started on ‘wet cutting.’ You think that’s not slowing down progress? We’re turning America into a museum.
Wake up people. This isn’t safety. It’s control.
It is of paramount importance to recognize that the hierarchical model of control, as promulgated by the Centers for Disease Control and Prevention and the Occupational Safety and Health Administration, constitutes a foundational paradigm in occupational hygiene. The emphasis on engineering controls over administrative controls and personal protective equipment is not merely a recommendation-it is an evidence-based imperative rooted in decades of epidemiological research and industrial case studies.
Furthermore, the assertion that respirator compliance drops precipitously during periods of elevated ambient temperature is not indicative of worker negligence, but rather a systemic failure in the design of protective gear and the absence of adaptive workplace protocols. The physiological burden imposed by P-100 respirators under thermal stress is well-documented in peer-reviewed literature from the Journal of Occupational and Environmental Hygiene, 2021, Volume 8, Issue 3.
Therefore, I submit that the solution lies not in merely enforcing compliance, but in redesigning the entire ecosystem of exposure mitigation to prioritize ergonomics, thermal comfort, and behavioral sustainability. Without this paradigm shift, all regulatory efforts remain fundamentally incomplete.
As a safety trainer in Mumbai, I’ve seen this exact scenario play out in textile mills and shipbreaking yards. Workers here don’t have wet-cutting machines. They don’t have exhaust hoods. They have rags and hope.
But here’s what changed: we started showing them videos of their own lungs-before and after. One man cried when he saw the scarring. He said, ‘I thought I was just coughing because of the heat.’
Training isn’t about rules. It’s about seeing yourself in the data. We made it visual. We made it personal. And suddenly, masks weren’t a chore-they became a shield.
Don’t wait for OSHA to come. Start today. Show your team their future. It’s not about cost. It’s about courage.
hmm
Love the Oregon stone shop example. That’s the blueprint. Not ‘just wear a mask’-but ‘let’s make this job safer so you don’t have to think about it.’
My uncle worked demolition in Detroit. Got diagnosed with asbestosis at 58. He never blamed his bosses. Said, ‘They didn’t know.’
That’s the tragedy. They didn’t know. Not because they were evil. Because nobody showed them.
So here’s what we do: if you’re in charge, take 10 minutes this week and show your crew that CDC video of the lung scan. Just 10 minutes. That’s all it takes to turn ignorance into action.
We can fix this. Not with fines. With facts.
the part about workers modifying their masks to breathe easier is so real i saw someone tape a straw to theirs last year
i just read this and i feel like crying. my dad was a drywall guy for 30 years. he never talked about it. now he’s on oxygen. i wish someone had told him. or told them.
thank you for writing this
There’s something deeply human here that gets lost in the data.
These aren’t just statistics. They’re fathers who can’t play with their kids because they’re out of breath. They’re mothers who can’t carry groceries. They’re people who spent their lives building things-only to have their own bodies become ruins.
Prevention isn’t just about engineering. It’s about dignity.
And dignity doesn’t come from a regulation. It comes from seeing someone and saying: ‘You matter more than the deadline.’
That’s the real hierarchy of control.
Everything else is just noise.
This is what happens when you let weak-minded liberals dictate how men should work. Real men don’t need wet saws or fancy vacuums. They need grit. They need to endure.
My country doesn’t have OSHA. We have men who show up and do the job. No complaints. No hand-holding. No masks.
Why should America be any different? You want to protect workers? Don’t coddle them. Make them stronger.
These diseases are nature’s way of filtering out the weak. Let them fall. The strong will survive.
And if you’re too fragile to breathe dust? Then you shouldn’t be in this line of work.
Stop treating men like children.
Write a comment