Switching from brand-name drugs to generics is supposed to save money without sacrificing results. For millions of people, it works perfectly. But for others, the story doesn’t end when the prescription fills. What happens after six months? A year? Five years? That’s where things get complicated.
Why Switching to Generics Feels Like a No-Brainer
Generic drugs cost a fraction of their brand-name counterparts. A statin that used to run $400 a month can drop to $4 with a generic. That’s not just savings-it’s access. In the U.S., generics make up 90% of all prescriptions filled. The math is simple: lower prices mean more people can afford their meds. And for many, that’s life-changing. But here’s the catch: affordability doesn’t always mean safety over time. The FDA says generics are bioequivalent. That means they deliver the same active ingredient at the same rate and amount as the brand. The standard? The drug’s concentration in your blood must fall between 80% and 125% of the brand’s levels. Sounds tight, right? It’s not. That 45% window is wide enough to create real differences in how your body responds-especially if you’re taking the drug every day for years. Think of it like this: two cars might both get 30 miles per gallon, but one sputters in cold weather, the other doesn’t. Same fuel. Different performance.The Hidden Risk: More Than Just the Active Ingredient
Generics have the same active ingredient. But they don’t have to match the brand’s inactive ingredients-the fillers, dyes, coatings, and binders. These don’t treat your condition. But they can affect how the drug is absorbed, how it tastes, even how your body reacts to it over time. A 2021 study in JAMA Internal Medicine found that generic drugs made in India had 27% more severe adverse events-like hospitalizations or death-than those made in the U.S. The difference? Not the active drug. The fillers. The manufacturing process. The quality control. And it’s not just about where it’s made. The same generic drug, made by two different companies, can have different effects. One patient on generic metoprolol succinate saw their heart rate spiral out of control after switching. When they went back to the brand, stability returned. Both met the FDA’s bioequivalence rules. But one version worked better for their body.Chronic Conditions Are the Real Test
For short-term use-like an antibiotic or a painkiller-generics are almost always fine. But for chronic conditions? That’s where long-term follow-up matters most. Take epilepsy. A 2013 study found that changing the pill’s color or shape during a generic switch reduced how long patients stayed on the drug by 35%. Why? Because patients got confused. They thought the new pill wasn’t the same. Some stopped taking it. Others took extra doses out of fear. Both choices are dangerous. Same with blood thinners like warfarin. Even tiny changes in how the drug is absorbed can mean the difference between a clot and a stroke. A 2022 IQVIA report shows only 63% of warfarin prescriptions use generics-because doctors know the risks. Even statins, which are generally safe as generics, show mixed results. One study found 77% adherence with generics versus 71% with brands. That’s good. But another study showed no difference in heart attack rates over five years. So which is it? The truth? It depends on the person. And the manufacturer. And how often they switch.
Switching Too Often Is the Silent Killer
One switch? Usually okay. Three switches in a year? Dangerous. A 2018 American Heart Association study found that patients who switched generic manufacturers three or more times in 12 months had a 40% higher risk of adverse events. Why? Because each switch introduces a new formulation. New fillers. New coatings. New absorption rates. Your body doesn’t get time to adapt. Pharmacies don’t always tell you when the generic changes. Insurance plans force switches to cut costs. You get a new bottle. Same pill name. Different color. Different shape. You don’t think twice-until you start feeling off. A 2020 University of Pittsburgh survey found that 61% of patients worried when their pill looked different. And 22% of them cut back on doses because they weren’t sure it was the same drug.What Works: A Smart Strategy for Long-Term Success
You don’t have to avoid generics. But you need a plan. Here’s what works, based on real-world evidence:- Start with stability. If your condition is well-controlled on a brand-name drug for at least six months, don’t switch unless you have to.
- Once you switch, stick with it. Find a generic manufacturer that works for you-and stay with that brand. Ask your pharmacist: “Which company makes this?” Write it down.
- Monitor closely for three months. Keep a log: energy levels, side effects, symptoms. If something changes, don’t wait. Call your doctor.
- Never let your pharmacy switch manufacturers without telling you. Ask for a written notice if your generic changes. If they won’t give it, switch pharmacies.
- For narrow therapeutic index drugs (like warfarin, levothyroxine, or seizure meds), avoid multiple switches. These drugs leave no room for error.
What Doctors and Pharmacies Should Be Doing
Most don’t. Only 35% of U.S. health systems track which generic manufacturer you’re on in your electronic record. That’s a problem. If you’re admitted to the hospital and your meds change, no one knows what you’ve been taking for the last two years. The American College of Physicians recommends that patients on chronic meds should be switched to a generic only once-and then kept on the same version. No more. And here’s the kicker: your doctor needs to talk to you about this. Not just hand you a script. Have a conversation. Ask: “Is this generic the same as the one I was on before?” “Has this version caused problems for other patients?”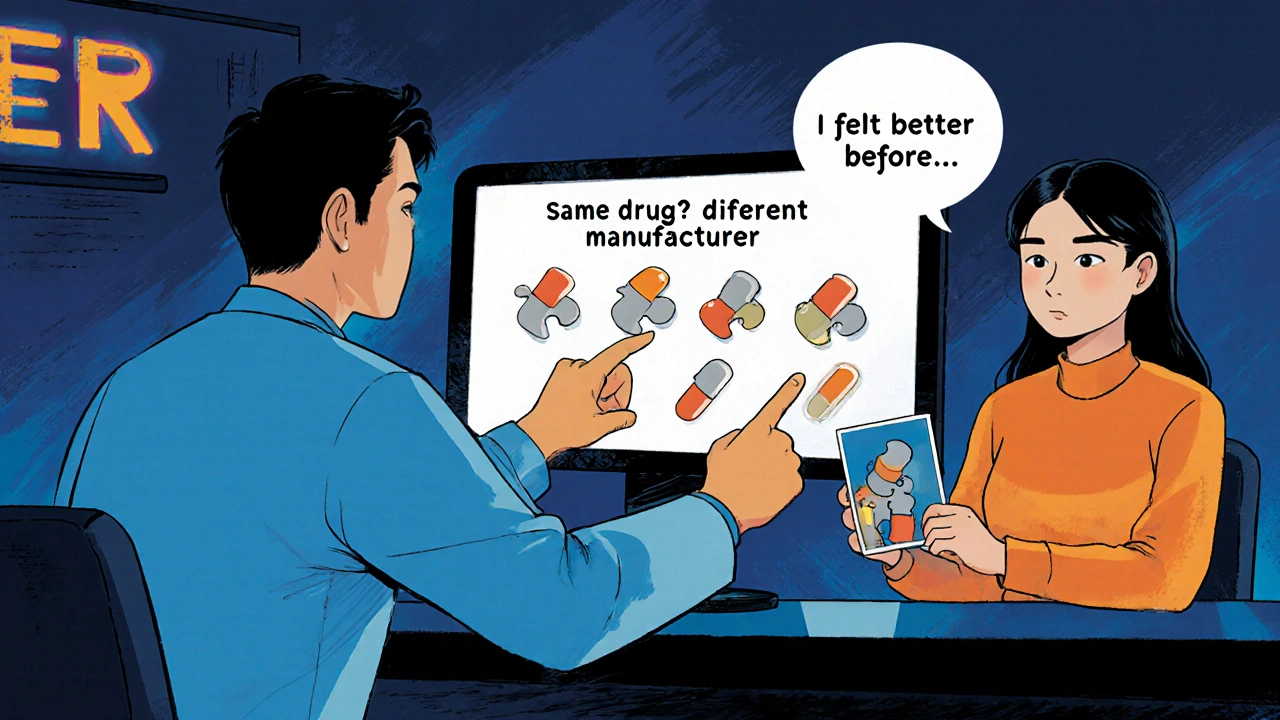
What You Can Do Today
You don’t need to wait for policy changes. Start with these steps:- Check your pill bottle. Note the manufacturer name (it’s printed on the side).
- Take a photo of your pill-front and back-so you remember what it looks like.
- Ask your pharmacist: “Is this the same manufacturer as last time?” If not, ask why.
- Track your symptoms for 30 days after any switch. Use a notes app or a paper journal.
- If you feel worse, don’t assume it’s ‘just in your head.’ Go back to your doctor with your notes.
The Bigger Picture: Cost vs. Long-Term Health
Generics saved $1.67 trillion in the U.S. between 2008 and 2017. That’s huge. But a 2015 study found that 64% of the time, switching to generics didn’t save money overall. Why? Because more people ended up in the ER. More hospital stays. More follow-up visits. The real cost isn’t the pill. It’s the consequence of a poorly managed switch. The FDA is starting to catch up. In 2023, they began requiring 36 months of stability data for generics used in chronic conditions. That’s progress. But it’s not enough. We still don’t know the long-term effects of contaminants found in some generics-like DNA-damaging chemicals-that might only show up after 7-10 years of daily use.Final Thought: Generics Are Tools, Not Guarantees
Generics aren’t bad. They’re essential. But they’re not all the same. And your body isn’t a lab test. It’s a living system that responds to subtle changes over time. If you’re on a generic for a chronic condition, don’t assume everything’s fine just because it’s cheaper. Stay alert. Stay informed. Stay consistent. Your long-term health depends on it.Are generic medications always safe for long-term use?
Most generics are safe and effective. But safety over decades depends on consistent manufacturing quality and stable formulations. Some patients-especially those on narrow therapeutic index drugs like warfarin or levothyroxine-experience changes in effectiveness or side effects after switching manufacturers. Long-term studies are still limited, so ongoing monitoring is key.
Can switching to a different generic cause health problems?
Yes. Even if two generics meet FDA bioequivalence standards, differences in inactive ingredients or manufacturing processes can affect how your body absorbs the drug. Patients with epilepsy, heart conditions, or thyroid disorders have reported worsening symptoms after switching between generic manufacturers. The risk increases with multiple switches in a short time.
How do I know if my generic medication has changed?
Check the pill’s shape, color, and imprint code. Compare it to your last bottle. Look for the manufacturer name printed on the tablet or packaging. If it’s different, ask your pharmacist. Many pharmacies don’t notify you when the generic changes, so it’s up to you to notice.
Should I ask my doctor to prescribe a specific generic manufacturer?
Yes-if you’ve found one that works well for you. Some doctors will write “Dispense as written” or “Do not substitute” on the prescription. You can also ask your pharmacist to order the same brand each time. It may cost more, but for chronic conditions, consistency can prevent serious complications.
Are generics made in India or China less safe?
Not all generics from these countries are unsafe, but studies have shown higher rates of severe adverse events linked to certain manufacturers there. The issue isn’t geography-it’s quality control. Some U.S.-made generics have issues too. The key is tracking which manufacturer you’re on and reporting any side effects. Don’t assume origin equals safety.
What should I do if I feel worse after switching to a generic?
Don’t ignore it. Document your symptoms: when they started, what they are, and how severe. Bring your pill bottles to your doctor. Ask: “Could this be related to the generic switch?” Request to return to your previous version. Many patients find relief simply by going back to the formulation that worked before.
Do insurance plans force generic switches?
Yes. Pharmacy benefit managers (PBMs) often change which generics are covered to cut costs. You might get a new bottle without warning. Ask your insurer for a list of preferred generics and whether they change frequently. You can request a formulary exception if a specific generic works better for you.
Is there a way to track which generic manufacturer I’m using?
Yes. Keep a simple log: date, drug name, manufacturer, pill appearance. Take a photo of each new bottle. Some apps like Medisafe or MyTherapy let you track medication changes. If your doctor uses an electronic health record, ask them to note your preferred manufacturer in your file.


12 Comments
I switched my statin to generic and felt like a zombie for two weeks. Went back to brand. Energy came back. No doctor even asked if I noticed a difference. Why do they assume we're all the same?
This is so real 🙌 I've been on the same generic levothyroxine for 4 years. Same manufacturer. Same pill. My TSH is perfect. But when they switched me to a different one last year? Heart racing, insomnia, the whole mess. Now I insist on the same brand. Pharmacy hates me but my thyroid loves me 😎
Man, I used to think generics were just cheap knockoffs. Then my grandma went on a generic blood thinner and ended up in the ER. Turned out the new batch had a different filler that messed with her absorption. She's fine now, but we learned the hard way: don't just trust the label. Check the manufacturer. Take pics of the pills. Write it down. Your life might depend on it.
As a clinical pharmacist, I've seen this pattern repeatedly. The FDA bioequivalence standard is a statistical average-not a guarantee for individual physiology. Patients on narrow therapeutic index drugs require individualized management. We must advocate for consistent formulations, not cost-driven substitutions.
India makes the best generics in the world bro. You americans are just paranoid. My cousin works in a pharma plant in Hyderabad and they follow WHO standards. Your doctors are just trying to keep you dependent on expensive brands. Stop being sheep and trust science!
THE GOVERNMENT IS HIDING THE TRUTH. Generics are laced with nanotech to track us. That’s why your pill changes color-different chips. My neighbor’s wife got dizzy after switching and now she can’t remember her kid’s birthday. They’re testing mind control on the poor. Wake up people!!! 🚨💣
The entire discourse here is fundamentally flawed. You're conflating bioequivalence with pharmacodynamic consistency. The 80-125% window is not a margin of error-it's a regulatory artifact designed to facilitate market competition. The real issue is the lack of longitudinal pharmacovigilance in post-market surveillance for chronic formulations.
I get why this feels scary. But I also know people who saved their homes because generics let them afford their meds. It’s not black and white. The key is awareness. Know your pill. Track your body. Talk to your pharmacist. You don’t have to be afraid-you just have to be smart.
From a pharmacokinetic standpoint, the inter-individual variability in Cmax and AUC is often underappreciated. The CYP450 polymorphisms in metabolizing enzymes can interact unpredictably with excipients, especially in polypharmacy regimens. This is why therapeutic drug monitoring remains critical in chronic care.
I heard the FDA lets them put asbestos in the coating if it's under 0.001%. That's why my hands get numb after taking my generic. They don't tell you because they're scared of lawsuits. I keep all my pill bottles in a freezer now. It stops the nanobots.
You people are so naive. If you can't afford the brand, you shouldn't be taking the medication at all. This isn't a grocery store. Medicine isn't a commodity. Your body is not a lab rat. Stop playing with your life because you want to save $12 a month.
I'm so glad someone finally wrote this. My mom switched generics three times in one year for her seizure meds. We didn't know until she had a seizure in public. Now we have a binder: pill photos, manufacturer names, dates. We even printed out the FDA’s list of approved manufacturers. It’s a pain-but it saved her life. You’re not overthinking. You’re being responsible.
Write a comment