Why Controlled Substance Verification Matters More Than Ever
Every time a pharmacist fills a prescription for oxycodone, hydrocodone, or Adderall, they’re not just dispensing medication-they’re acting as the last line of defense against diversion, overdose, and illegal distribution. In 2023, the DEA reported over 6,200 enforcement actions tied to improper verification of controlled substances. That’s not a small number. That’s a system breaking down at the pharmacy counter. And it’s not just about following rules-it’s about saving lives.
The stakes are real. A single mistake in quantity or directions can mean the difference between a patient getting the right dose and someone receiving 10 times what was prescribed. Or worse-someone getting a prescription that was never meant for them.
There’s no room for guesswork. The DEA, FDA, and state boards don’t just expect you to verify these prescriptions. They require it. And they’re watching.
The Seven Mandatory Elements of a Valid Prescription
You can’t verify what you don’t know to look for. Every controlled substance prescription-whether it’s a Schedule II like fentanyl patches or a Schedule IV like alprazolam-must contain seven specific elements. Missing even one can make the prescription invalid.
- Prescriber’s full name and address: No abbreviations. No "Dr. Smith, Portland"-it must be the full legal name and practice address as registered with the DEA.
- Date of issuance: For Schedule II drugs, the date must be today. No backdating. For Schedules III-V, it can be up to six months old, but no more.
- Patient’s full name and address: Middle initials matter. "J. Smith" is not the same as "John Smith" if the DEA file says "John".
- Drug name and strength: "Hydrocodone 10mg" is not the same as "Hydrocodone 7.5mg". Strength must match the DEA’s approved nomenclature.
- Dosage form: Is it a tablet? Capsule? Liquid? Extended-release? This determines how it’s counted and dispensed.
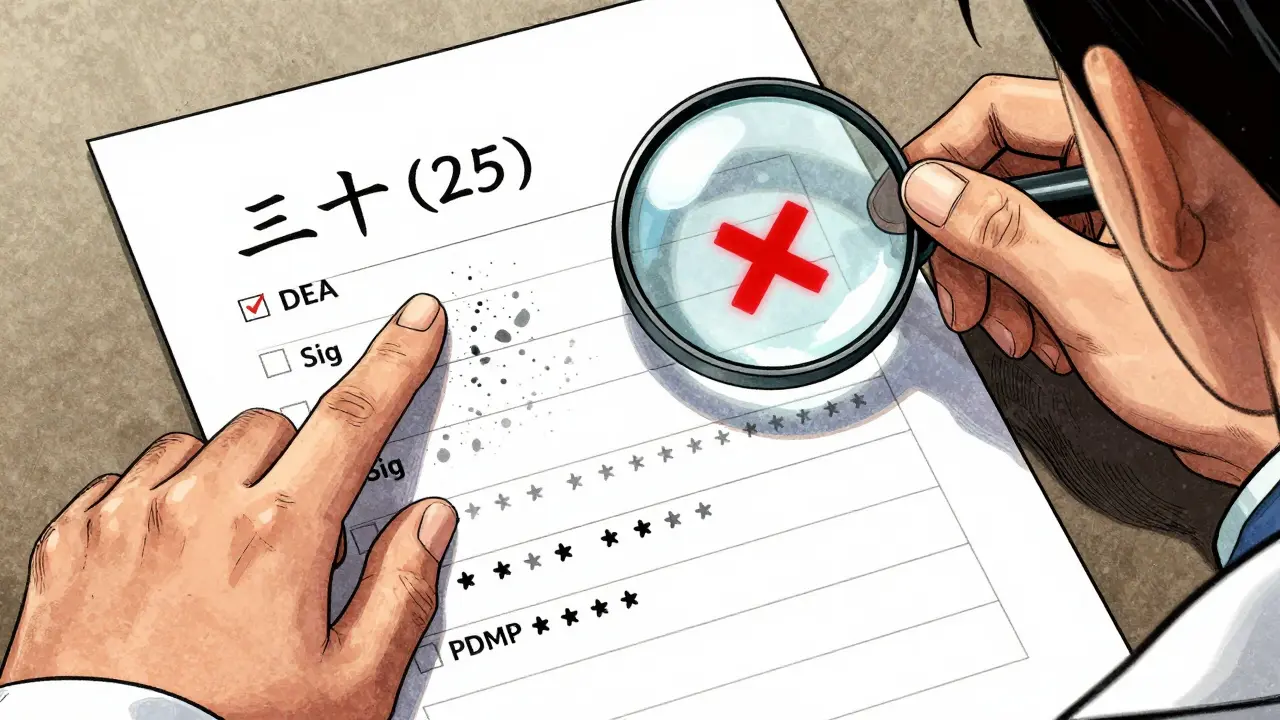
- Quantity prescribed: This is where most errors happen. You must check both the written number and the numeric value. "Thirty (30) tablets"-if it says "25" numerically, it’s invalid.
- Directions for use (sig): "Take one by mouth every 6 hours as needed for pain"-not "1 q6h PRN pain". Abbreviations are allowed, but only if they’re standard and unambiguous.
If any of these are missing, unclear, or mismatched, you cannot fill the prescription. Period.
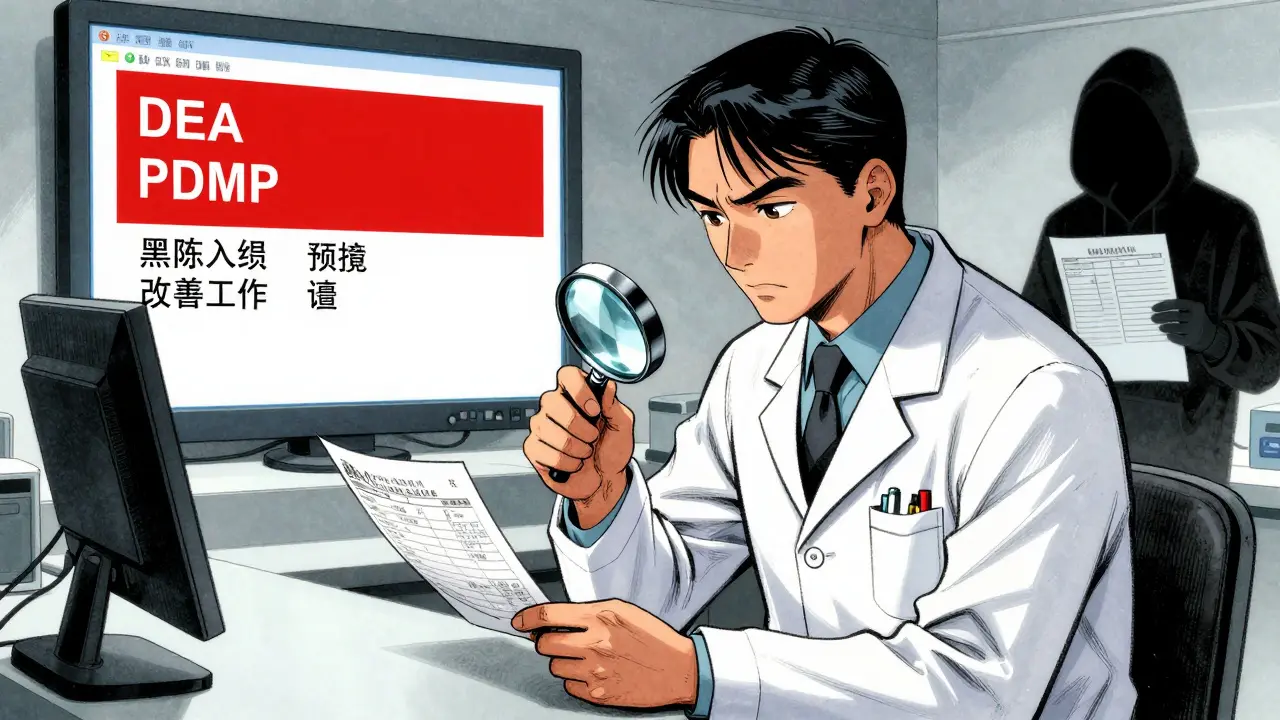
Verifying the DEA Number: The 3-Step Math Test
DEA numbers aren’t random. They’re coded. And if you don’t check them, you’re not just being lazy-you’re risking your license.
A valid DEA number looks like this: AB1234567. Here’s how to verify it:
- Second letter must match the prescriber’s last name initial. If the prescriber is Dr. Smith, the second letter must be "S". If it’s "A", it’s fake.
- Add the 1st, 3rd, and 5th digits. In AB1234567, that’s 1 + 3 + 5 = 9.
- Add the 2nd, 4th, and 6th digits, then multiply by 2. That’s 2 + 4 + 6 = 12. Multiply by 2 = 24.
- Add the two totals: 9 + 24 = 33. The last digit (3) must match the 7th digit of the DEA number.
If it doesn’t match? Don’t fill it. Call the prescriber. Report it to the DEA if it looks fraudulent. The DEA’s own 2021 study found this method catches 98.7% of fake DEA numbers. That’s not luck-that’s math.
Quantity Verification: The #1 Source of Errors
According to CMS data from 2022, 2% of all Medicaid prescription rejections were because the written quantity didn’t match the numeric quantity. That’s one in every 50 prescriptions. And those aren’t just clerical errors-they’re safety risks.
Here’s how to catch them:
- Always compare the written word and the number side by side. "Twenty (20)"? Good. "Twenty (15)"? Red flag.
- Watch for tampered prescriptions. Look for smudges, erasures, or numbers written over printed boxes. Since 2008, DEA requires security paper with microprinting and asterisk-bordered quantity fields. If it’s on plain paper? Be suspicious.
- Check refill limits. Schedule II drugs can’t be refilled. Schedule III-V can have up to five refills in six months. If a prescription says "Refill 3" but it’s a Schedule II, it’s invalid.
And don’t forget: if the quantity is unusually high-for example, 120 hydrocodone tablets for a 7-day supply-that’s a red flag. Cross-check with the directions. If the sig says "take one daily," that’s 30 tablets for 30 days. 120 tablets means either a 4-month supply or a red flag for abuse.
Directions (Sig) Verification: Don’t Assume Anything
"Take one by mouth every 4 to 6 hours as needed" is clear. But what about "1 q4-6h PRN"? Is that acceptable? Yes-if it’s standard. But "1 qid"? That’s ambiguous. Is it four times a day? Or four tablets at once? Pharmacists have been sued over this.
Here’s your checklist:
- Confirm the frequency matches the quantity. If 60 tablets are prescribed and the sig says "take two three times daily," that’s 6 per day-10 days’ supply. That’s fine. But if it’s 60 tablets and "take two every hour," that’s 48 per day-1.25 days. That’s dangerous.
- Watch for dangerous abbreviations. "QD" (daily) is still allowed, but "QID" (four times daily) is better written as "four times daily". Avoid "U" for unit-it can be mistaken for "0".
- For opioids, match the sig to CDC conversion factors. If a patient is on 40 mg of hydrocodone daily and the new script is for 15 mg of oxycodone, that’s not equivalent. Oxycodone is 1:1 with hydrocodone, but if the patient is on 60 mg of methadone, you need to use the 10:1 conversion ratio for 41-60 mg/day ranges. Get this wrong, and you could cause respiratory depression.
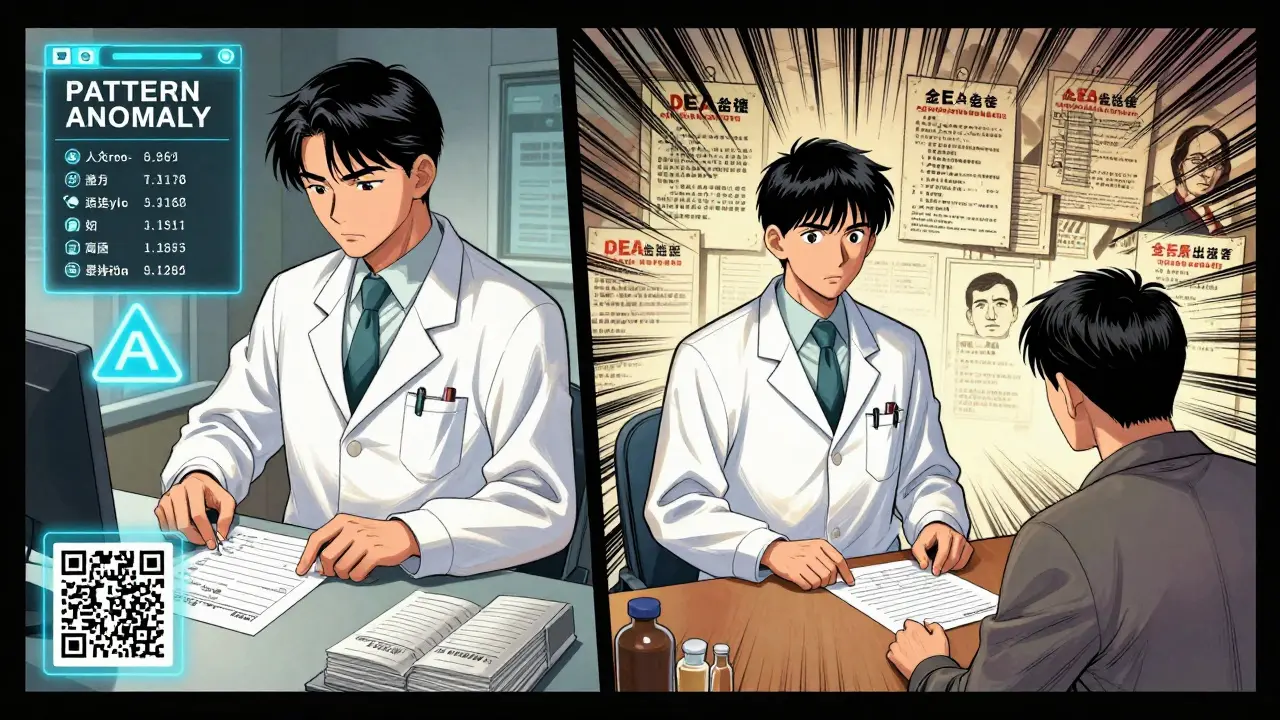
Using PDMPs: Your Most Powerful Tool-If You Use It Right
Forty-nine states require pharmacists to check the Prescription Drug Monitoring Program (PDMP) before dispensing controlled substances. But here’s the catch: not all PDMPs are equal.
As of January 2024:
- 27 states require real-time data (updated within 5 minutes).
- 18 states allow 24-hour updates.
- 4 states only update weekly.
That means if you’re in California and you check a prescription, you might be seeing data from yesterday. In Tennessee? You’re seeing it live.
What to look for in the PDMP:
- How many controlled substance prescriptions has this patient filled in the last 30 days?
- Are they getting opioids from multiple prescribers?
- Is the quantity or frequency unusual compared to their history?
- Has this prescriber been flagged for high-volume prescribing?
Pharmacists using PDMPs correctly report a 37% drop in suspicious prescriptions. But if you only check it once a week? You’re missing the point. Check it every time. Every. Single. Time.
Manual vs. Electronic Verification: What Works Best
Independent pharmacies still rely mostly on manual checks. Chain pharmacies use automated systems. Which is better?
Manual verification: You see everything. You catch the smudged number, the illegible sig, the mismatched DEA letter. But it’s slow. And humans make mistakes. University of Florida research found manual verification has an 18.7% error rate.
Electronic systems: They auto-check DEA numbers, flag quantity mismatches, pull PDMP data instantly, and validate DSCSA product identifiers. Accuracy? 99.2%. But they cost $15,000 to $50,000 to install. And they’re useless if you don’t train staff to interpret the alerts.
The best approach? Combine both. Use automation to catch the obvious errors, then use your judgment for the gray areas. If the system flags a script, don’t just click "approve." Ask: Why did it flag it? What’s the context?
What Happens When You Get It Wrong
In 2023, the DEA increased civil penalties to $758,574 per violation. That’s not a typo. That’s more than most pharmacies make in a year.
License revocation? Common. Criminal charges? Happens. In 2022, a pharmacist in Ohio was charged with conspiracy after filling 200+ oxycodone prescriptions from a single doctor who was later convicted of racketeering. The pharmacist claimed they "didn’t know." The court didn’t care.
And it’s not just about punishment. Your reputation is on the line. Patients trust you. If they find out you filled a script that should’ve been flagged, they’ll take their business elsewhere. And they’ll tell others.
Pro Tips from the Front Lines
Here’s what experienced pharmacists do differently:
- Keep a printed checklist taped to your workstation: DEA, name, date, quantity, sig, PDMP, security paper. Check each box as you go.
- Use a magnifying glass for microprinting. It’s not optional. It’s required.
- Call the prescriber if anything feels off-even if the system says it’s valid. You’re the pharmacist. You have the final say.
- Document everything. If you called the doctor, wrote a note, or refused a script, log it. In a dispute, your notes are your shield.
- Use NABP’s PMP InterConnect. It’s the most reliable PDMP aggregator. Rated 4.7/5 by pharmacists. Reduces verification time by nearly 40%.
The Future: QR Codes and AI
By 2026, every controlled substance prescription in the U.S. must include a QR code linked to a unique product identifier under DSCSA rules. That means you’ll scan a code and instantly see the drug’s entire chain of custody-from manufacturer to pharmacy.
And the DEA is testing AI tools that analyze prescribing patterns. If a doctor writes 100 scripts for 90 mg of methadone in a week? The system will flag it. You’ll get a notification before you even open the script.
These aren’t sci-fi ideas. They’re coming. And if you’re not ready, you’ll be left behind.
Final Rule: When in Doubt, Don’t Fill It
You don’t need to be a detective. But you do need to be careful. If a prescription looks off, smells wrong, or just doesn’t feel right-stop. Call the prescriber. Check the PDMP again. Ask a colleague. Use the DEA’s free OSCAR training module. Do whatever it takes.
Because in this job, your attention to detail isn’t just professional. It’s moral. And it’s the only thing standing between a patient and harm.

14 Comments
This is the most overcomplicated waste of time I've ever read. If you're actually checking every single one of these steps on every script, you're working 12-hour days just to fill 20 prescriptions. The system is broken, not the pharmacist.
There's a quiet dignity in the act of verifying a prescription-not as a bureaucratic hurdle, but as a sacred ritual of accountability. Each digit, each letter, each microprint is a thread in the fabric of trust between healer and healed. When we reduce this to checkboxes and automated alerts, we risk forgetting that medicine is not a transaction-it is a covenant. The DEA may enforce rules, but it is the pharmacist’s conscience that upholds the humanity of care.
I’ve had patients cry because I refused a script that looked sketchy. One guy said, 'I just need to get through the week.' I didn’t fill it. He came back two days later with a letter from his doctor. We cried together. This job isn’t about rules-it’s about being the person who says 'no' so someone else doesn’t have to die.
DEA math check? Bro, just scan the QR code when it rolls out next year and move on.
Seven elements? Please. In India we verify with a glance and a gut. Western obsession with documentation is just performative compliance. Real medicine doesn't need checklists-it needs intuition
I work in Texas and let me tell you if you dont follow every single one of these rules you are asking for trouble. This is AMERICA we dont do half measures here and if you think some foreign country knows better you are delusional
i just wanted to say thank you for writing this. i’m a new pharmacist and i was terrified i’d mess up. this made me feel like maybe i can actually do this right. also sorry for typos i’m typing on my phone while my toddler screams in the background 😅
2% error rate? That’s not a problem. That’s a feature. If every script was perfect we wouldn’t need pharmacists. We’d need robots. And robots don’t get fired when they refuse a script. Humans do.
I’ve worked in Mumbai and now in Chicago. The rules are different, but the heart isn’t. When a mother asks if her child’s ADHD med is safe, it doesn’t matter if the DEA number is perfect. What matters is that you listened. This guide helps-but don’t let it make you forget why you became a pharmacist.
Oh wow, look who’s writing a textbook. I bet you also check the ink viscosity on the prescription paper and hum the national anthem while scanning the QR code. Next you’ll be measuring the humidity in the pharmacy to ensure optimal opioid stability. 🤡
I used to do the manual math on DEA numbers. Then I got an electronic system. It caught a fake script I would’ve missed because the prescriber’s last name started with 'Mc' and the second letter was 'C'-but the DEA system registered it as 'M'. The system didn't care about my assumptions. It just knew the math. Sometimes the machine sees what we're too tired to.
The DSCSA implementation timeline and the interoperability of PDMPs remain suboptimal across state lines. The current regulatory architecture exhibits significant fragmentation, which introduces systemic inefficiencies in controlled substance verification protocols. Further standardization is required to achieve compliance at scale.
This isn’t just about pills. 🌱 It’s about dignity. It’s about the single mom who needs her Adderall to keep her job. It’s about the veteran who’s one bad script away from oblivion. It’s about the pharmacist who shows up at 5 AM, tired, but still checks the microprint. You’re not just a dispenser. You’re a guardian. And yeah, I cried reading this. 🥹
In South Africa, we do not have the luxury of automated systems or real-time PDMPs. We rely on training, intuition, and the courage to say no. Your guide is thorough, but it assumes infrastructure that does not exist in many parts of the world. Perhaps the real lesson is not how to verify-but how to endure.
Write a comment