Switching a patient from a brand-name NTI drug to a generic version isn’t just a pharmacy transaction-it’s a clinical decision that requires clear, honest communication. NTI drugs are among the most dangerous medications to switch without proper oversight. Even tiny changes in blood levels can lead to seizures, blood clots, or thyroid failure. Yet, many patients are never told why their pill looks different, or what to watch for after the switch.
What Makes NTI Drugs So Different?
NTI stands for Narrow Therapeutic Index. These drugs have a razor-thin line between working and causing harm. Take warfarin, for example. The goal is to keep the INR between 2 and 3. If it drops to 1.8, the patient could develop a clot. If it climbs to 3.5, they could bleed internally. Digoxin? A level above 0.9 ng/mL can trigger dangerous heart rhythms. Phenytoin? One point above 20 mcg/mL can cause dizziness, tremors, or worse.
The FDA requires stricter testing for generic versions of these drugs. While regular generics must match brand-name drugs within 80%-125% of the active ingredient, NTI generics must hit 90%-111.11%. For drugs like levothyroxine, the bar is even higher: AUC must be within 95%-105%. This isn’t just bureaucracy-it’s life-or-death precision.
Why Do Patients Worry About Generic NTI Drugs?
Patients aren’t being irrational. They’ve heard stories. A 2017 survey found that 8-12% of well-controlled epilepsy patients had seizures after switching from brand to generic antiepileptics. Another study showed that 60% of pharmacists still hesitate to substitute NTI generics-even though 94% believe they’re safe. That hesitation gets passed down to patients.
Some patients remember the time their thyroid meds changed and they felt tired for weeks. Others had a loved one hospitalized after a switch. These aren’t myths-they’re real experiences, even if the cause wasn’t always the generic itself. The fear sticks because the stakes are so high.
What You Must Say to Patients
Don’t say, “It’s the same thing.” That’s not enough. Don’t say, “The FDA says it’s okay.” That sounds like a cop-out.
Instead, say this:
- “This generic version has been tested to deliver the exact same amount of medicine into your bloodstream as the brand. The FDA requires stricter testing for drugs like this because even small differences matter.”
- “I prescribe this same generic to my own family members. I trust it because the data shows it works just as well.”
- “We’re going to check your blood levels in 7 to 10 days to make sure everything’s still on target. That’s just how we keep you safe.”
Use the word “we.” It turns a pharmacy decision into a team effort. Patients feel less like they’re being handed a random pill and more like they’re part of a care plan.

When to Avoid Switching
Not every patient should switch. Avoid substitution if:
- The patient has been stable on the brand for more than a year and has no history of dosing issues.
- The patient is elderly, has kidney or liver disease, or takes multiple medications that interact with the NTI drug.
- The patient has had a bad reaction to a previous generic switch-even if it was years ago.
- The patient expresses strong distrust or anxiety about the switch.
In these cases, staying on the brand is safer than pushing for cost savings. Insurance companies may push for generics, but your job is to protect the patient-not the bottom line.
What States Require
Twenty-seven states have laws that affect how NTI drugs can be switched. Fourteen of them require written patient consent before substitution. Some states require pharmacists to notify the prescriber. Others ban substitution entirely for certain drugs.
Before you switch a patient, check your state’s rules. You can’t assume the pharmacy will handle it. If your state requires consent, get it in writing. Document it in the chart: “Patient counseled on therapeutic equivalence of generic [drug name], advised of need for monitoring INR within 5 days, and provided written materials.”
Monitoring Is Non-Negotiable
After a switch, you can’t just wait for the patient to call if something’s wrong. Set up a plan:
- For warfarin: Check INR within 3-5 days.
- For phenytoin or carbamazepine: Check serum levels within 7-10 days.
- For levothyroxine: Check TSH in 4-6 weeks.
- For digoxin: Check levels and symptoms within 7 days.
Don’t wait for symptoms. These drugs don’t always warn you before they cause harm. A patient might feel “fine” while their INR climbs into danger zone. Routine checks are the only way to catch it early.
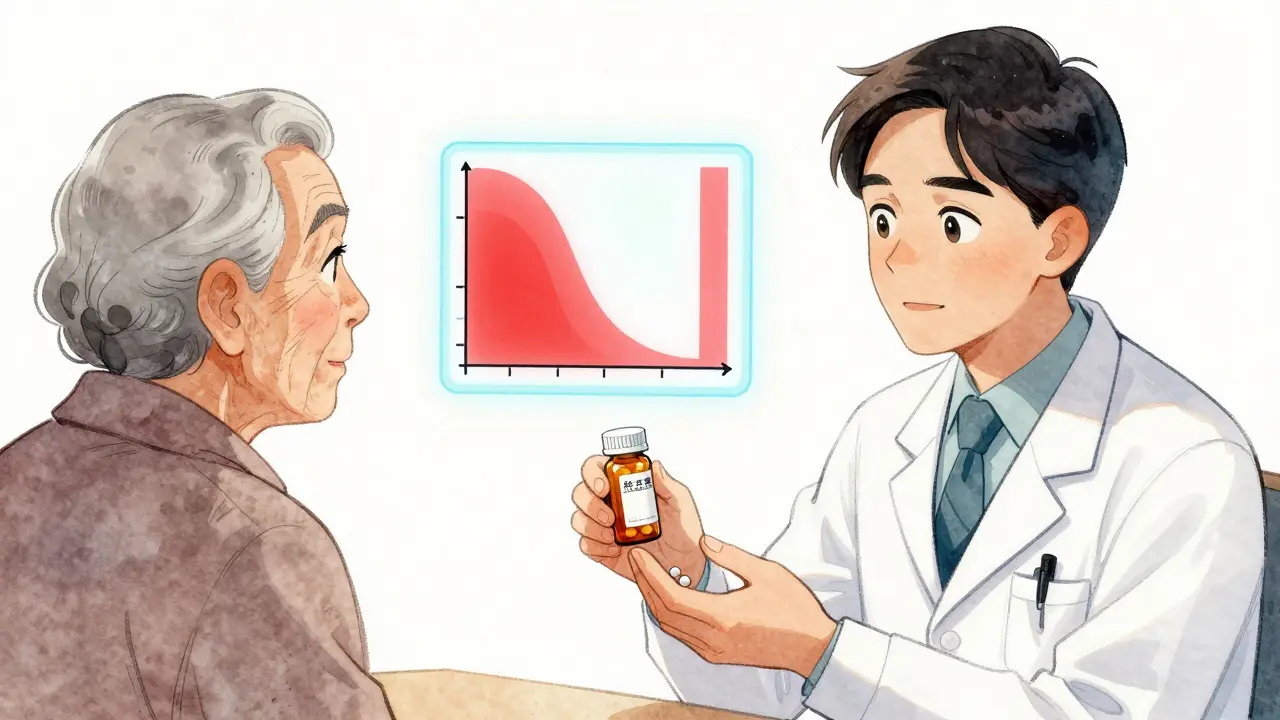
Use Visual Aids and Teach-Back
A 2023 study found that pharmacists who used simple charts or diagrams during counseling saw 42% higher adherence rates. Show a patient a graph of the therapeutic window-how the safe range is a narrow band. Point to it. Say, “This is where we need you to stay.”
Then, use the teach-back method. Ask: “Can you tell me in your own words why we’re checking your blood in a week?” If they can’t, explain again. Don’t assume they understood because they nodded.
Patients remember what they say, not what they hear.
What to Do If Problems Arise
Even with perfect communication and monitoring, some patients will have issues after a switch. That doesn’t mean the generic failed. It might mean their body reacted differently to a new filler or coating. Or maybe they missed a dose. Or maybe their kidney function changed.
Here’s what to do:
- Don’t panic. Most cases are manageable.
- Check the drug level immediately.
- Compare it to their baseline on the brand.
- If it’s outside range, consider switching back or adjusting the dose.
- Report the event to MedWatch-even if you’re not sure it was caused by the switch.
The FDA has logged over 1,200 adverse events tied to NTI drug switches since 2019. Most weren’t proven to be caused by the generic-but reporting helps identify patterns. Your report could help prevent the next incident.
Why This Matters Beyond Cost
NTI generics cost less. That’s true. But the real value isn’t in the price tag. It’s in access. Millions of patients can’t afford brand-name versions. Without generics, they go without treatment. That’s worse than any risk from substitution.
The goal isn’t to eliminate brand-name drugs. It’s to make generics safe, trusted, and widely used. That only happens when providers stop treating NTI switches as a technicality and start treating them as a personal commitment to patient safety.
Every time you take five minutes to explain, monitor, and follow up, you’re not just preventing a bad outcome. You’re rebuilding trust in the system. And that’s worth more than any savings on a prescription.

13 Comments
This post hits hard. I’ve seen patients crash after a switch-INR out of range, no warning. No one told them it wasn’t just a different pill. The FDA’s 90-111% range sounds precise, but bodies aren’t labs. One patient’s thyroid gland reacts differently to fillers. That’s not theory-that’s Tuesday in clinic.
We don’t talk enough about bioequivalence being population-based, not individual. What’s ‘safe’ for 95% of people can still kill the 5%. And when that 5% is your patient, ‘statistically sound’ doesn’t mean squat.
Doctors treat this like a formality. It’s not. It’s a risk assessment every single time. And if you’re not checking labs after a switch, you’re not practicing medicine-you’re playing Russian roulette with a prescription pad.
I’ve switched dozens of patients on levothyroxine. Always check TSH at 6 weeks. Never assume. Always document. The pharmacy handles the substitution, but the provider owns the outcome.
One of my patients cried when I told her we were switching her warfarin. Said her husband almost died after a generic switch years ago. I didn’t push. We kept the brand. Cost? $180 more a month. Her life? Priceless. Sometimes the right call isn’t the cheapest one.
That’s what this post gets-this isn’t about savings. It’s about trust. And once you break it, you might never get it back.
U guys in usa think u r so smart with ur fda rules but in nigeria we just give the pill and tell them to take it. no blood tests no consent no drama. u overthink everything. we save lives by simplicity. u waste time on paperwork while people die waiting for u to sign a form.
The 2017 epilepsy study is misleading. Most seizures were due to nonadherence or intercurrent illness. The generic wasn't the culprit. But you'll keep blaming the pill because it's easier than admitting your patients don't take meds properly
I work with refugees. Many don’t speak English. We use pictures. A pill bottle with a checkmark. A graph of the narrow band. We point. They nod. Then we ask them to show us the graph again. 90% get it right the second time.
Teach-back isn’t just good practice-it’s survival.
OMG YES. I just had a patient tell me she didn’t switch her phenytoin because she ‘felt weird’ after the last generic. I was like ‘thank you for speaking up’-and we stayed on brand. She was terrified. And you know what? She’s been stable for 8 months now.
It’s not about being right. It’s about being safe. And sometimes, safety means listening even when the data says you don’t have to.
It is imperative to underscore that the regulatory framework governing NTI generics is not merely a guideline; it is a codified, evidence-based standard designed to mitigate clinical risk. Failure to adhere to state-mandated consent protocols constitutes a breach of the standard of care, and may expose the prescriber to liability under tort law.
Furthermore, the utilization of teach-back methodology is not optional-it is a best practice endorsed by the Institute of Medicine and the Joint Commission. Documentation must be contemporaneous and specific.
Love this. Seriously. I used to think generics were just a cost thing. Then I had a patient on digoxin who got dizzy after a switch. We checked levels-she was at 1.4. Brand was 0.7. We switched back. She was fine. But I didn’t know to check until she came back in.
Now I don’t just say ‘it’s the same.’ I say ‘we’re watching you.’ And I mean it. That changes everything.
The pharmacokinetic variability of NTI generics is not adequately addressed by current FDA bioequivalence thresholds. The 90–111.11% AUC range is statistically acceptable but clinically insufficient for patients with polymorphic CYP450 metabolism, particularly in South Asian populations where CYP2C9 and CYP2C19 variants are prevalent. Without genotyping or therapeutic drug monitoring, substitution is an uncontrolled experiment.
Moreover, excipient differences-such as lactose content or dye composition-can trigger immune-mediated adverse reactions in susceptible individuals, a phenomenon rarely documented in post-marketing surveillance.
My grandma was on levothyroxine for 20 years. Brand only. When they switched her to generic, she got so tired she couldn’t walk to the mailbox. We switched back. She cried. Said she felt like herself again.
That’s not ‘patient anxiety.’ That’s her body telling us something. We don’t need more data. We need more listening.
People think this is about medicine. It's not. It's about control. The system wants you to believe generics are safe so you stop asking questions. But the truth? They're cheaper. And cheaper means more profit. Don't be fooled by the FDA logo.
Thank you for this. I’m a pharmacist in London, and we’re seeing more NTI switches due to NHS cost pressures. We’ve started using printed visual aids-simple, with the therapeutic window drawn as a narrow lane. Patients say it helps.
We also have a checklist: 1. Confirm patient understands 2. Confirm monitoring plan 3. Document consent 4. Notify prescriber if required. It’s taken 3 minutes extra per patient-but we’ve had zero adverse events since.
Write a comment