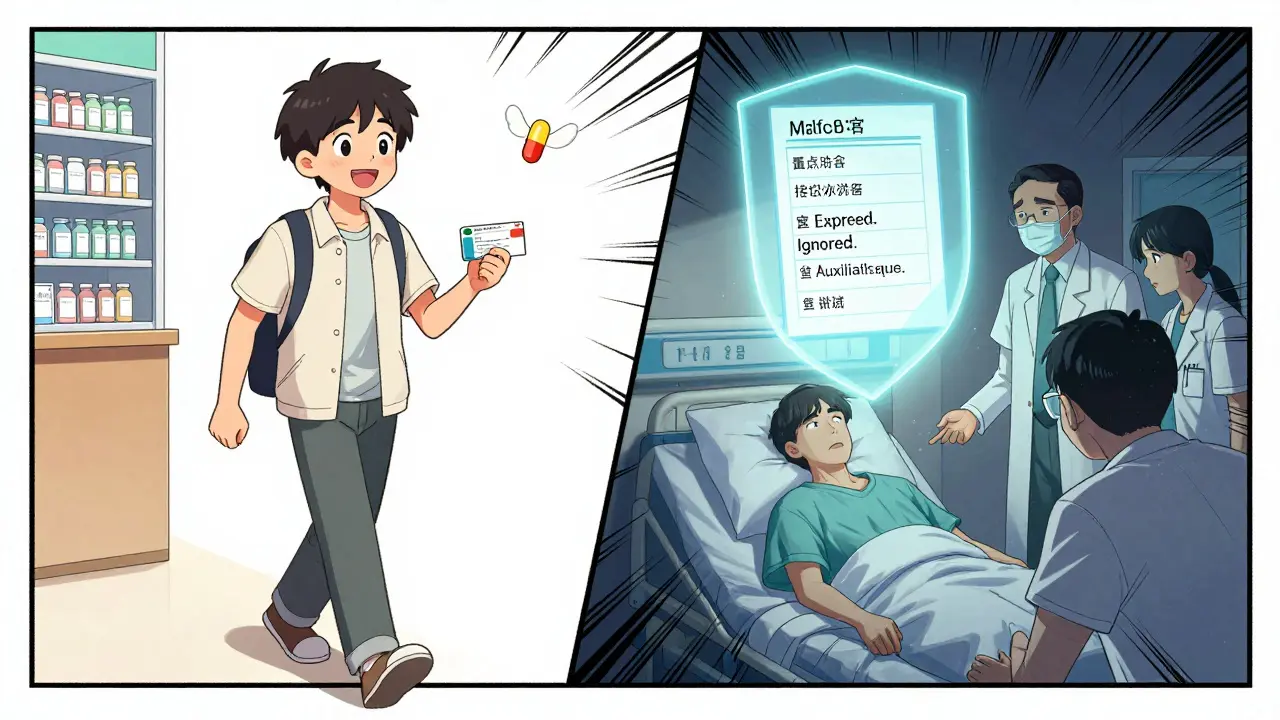
Every time you pick up a new prescription, you’re handed a small piece of paper that could mean the difference between getting better and ending up in the hospital. Prescription labels aren’t just paperwork-they’re your safety guide. But most people glance at them, shrug, and go on with their day. That’s a mistake. Around 79% of patients misread at least one part of their medication label, according to a major NIH study. And that’s not just about confusion-it’s about risk.
What’s on Your Prescription Label?
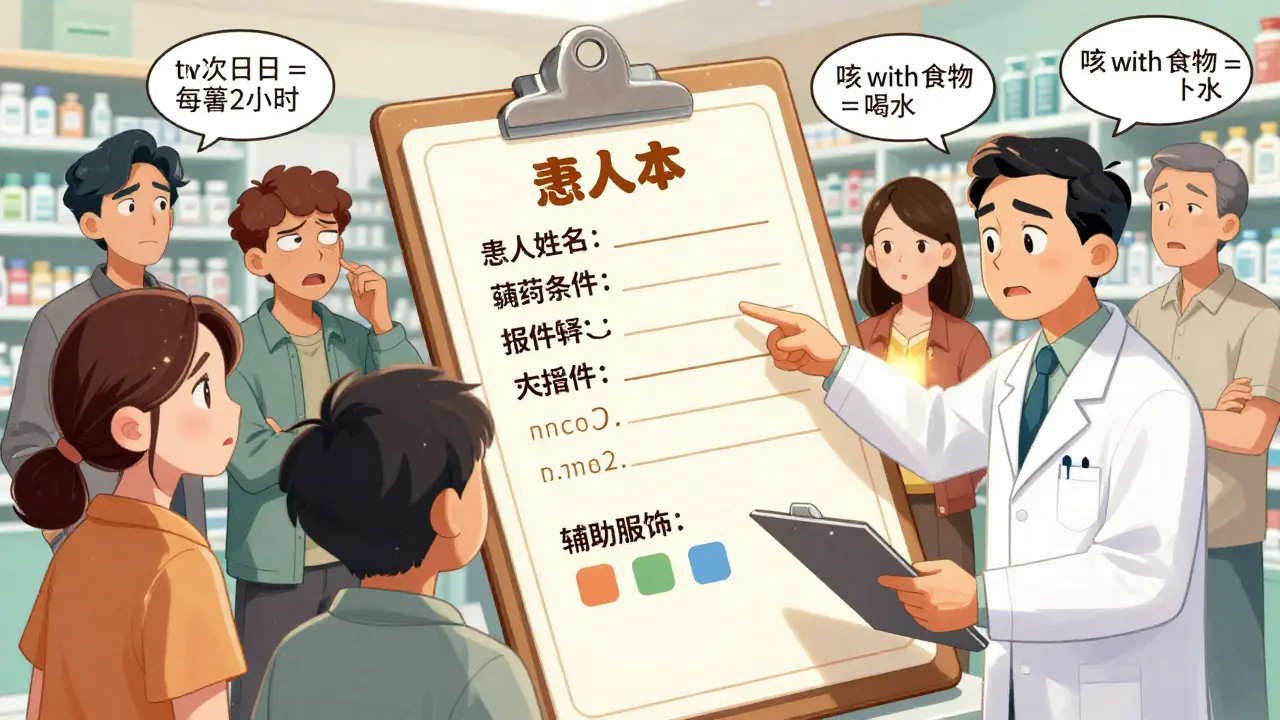
Your prescription label has twelve key pieces of information. If you don’t know what each one means, you’re flying blind. Here’s what you’re actually looking at:- Patient Name: This isn’t just for show. It stops someone else from accidentally taking your medicine. Always check that your full name matches exactly-no nicknames, no initials.
- Medication Name: You’ll see two names: the brand name (like Lipitor) and the generic name (like atorvastatin). The generic name is the actual drug. Knowing both helps you recognize the medicine if your pharmacy switches brands.
- Prescription Number (Rx#): This is your prescription’s ID. It’s how the pharmacy tracks your refill requests. Write it down or save it in your phone.
- Prescriber Name: Who ordered this? It could be your doctor, nurse practitioner, dentist, or even a vet if it’s for a pet. If you’re unsure why you’re taking it, call this provider.
- Medication Strength: This tells you how much of the drug is in each dose. For example, “20 mg tablets” means each pill has 20 milligrams. Mixing up 5 mg and 20 mg can be dangerous. Always compare this to your last prescription.
- Quantity: How many pills, milliliters, or grams did you get? If you got 30 pills but the label says “take one daily,” you should have enough for a month. If you got 10 pills for a 30-day supply, something’s off.
- Discard/Expiration Date: Most prescriptions expire one year after being filled. After that, the medicine may not work-or could break down into something harmful. Never take pills past this date.
- Instructions: This is the most misunderstood part. “Take twice daily” doesn’t mean every 12 hours-it means morning and night. “Take as needed” means only when symptoms happen, not every hour. The NIH found that 23% of people with low health literacy think “twice daily” means every two hours.
- Refill Info: How many more times can you get this without a new prescription? If it says “3 refills,” you can get it four times total (the original + 3 refills). Don’t wait until you’re out-call ahead.
- Auxiliary Labels: These are the small stickers: “Take with food,” “Avoid alcohol,” “Refrigerate,” or “May cause drowsiness.” These aren’t optional. Skipping “take with food” can wreck your stomach. Ignoring “avoid sunlight” can give you a bad burn.
- Pharmacy Info: Name, address, phone number. Save this. If you have questions, call them. Pharmacists are trained to explain labels. Don’t be shy.
Why Do People Get It Wrong?
It’s not your fault. Prescription labels were designed by pharmacists and regulators-not patients. They use terms like “q.i.d.” or “bid,” which most people don’t know. Even when labels are written in plain English, they’re still confusing.A study tested 400 people with different education levels. Those with low health literacy were more than twice as likely to misunderstand instructions-even when the wording was simple. One common mistake: thinking “take three times a day” means every eight hours. But if you take it at 7 a.m., 3 p.m., and 11 p.m., you’re sleeping through a dose. That’s not what the doctor meant.
Another big issue? Vague language. “Take as needed” sounds simple-but for someone with chronic pain, it’s unclear. Do you wait until the pain is unbearable? Or take it before it starts? Ask your pharmacist to clarify.
Seven Steps to Read Your Label Right
Before you leave the pharmacy, do this checklist. It takes two minutes. It could save your life.- Match the name: Is your full name spelled right? No typos, no missing middle names.
- Check the drug: Does it look like what you expected? If you’ve taken this before, compare the color, shape, and markings. If it looks different, ask why.
- Confirm the strength: Did they give you the same dose as last time? If you were on 10 mg and now it’s 20 mg, double-check with the pharmacist.
- Understand the instructions: Say them out loud. “I take one tablet in the morning and one at night.” If you’re unsure, ask: “Can you show me on a clock?”
- Read the auxiliary labels: Those little stickers? They’re there for a reason. If it says “avoid grapefruit,” don’t eat it. If it says “shake well,” shake it.
- Check the expiration date: Write it on your calendar. If it’s in six months, mark a reminder to dispose of it.
- Save the pharmacy number: Don’t just throw away the bag. Keep the label. Call them if you have questions-even at 10 p.m.

What to Do If Something Feels Off
You don’t have to guess. If the label doesn’t make sense, if the pill looks wrong, if the instructions contradict what your doctor said-speak up. Here’s what to do:- Call the pharmacy. Pharmacists are legally required to explain your prescription.
- Ask for a printed copy of the FDA-approved drug information sheet. It’s detailed, but clear.
- Request a consultation. Many pharmacies offer free 10-minute med reviews.
- Take a photo of the label with your phone. Compare it next time you refill.
It’s not rare to get the wrong medicine. The FDA tracks errors and finds that about 1 in every 5,000 prescriptions is filled incorrectly. Most of those mistakes happen because the label was misread-or not read at all.
What’s Changing on Prescription Labels
The system is getting better. In 2014, the FDA pushed for clearer labeling. No more Latin abbreviations. No more tiny print. Now, labels must use plain language like “take once a day” instead of “q.d.”Some pharmacies are going further. In 2022, Express Scripts tested QR codes on labels. Scan it, and you get a short video in your language showing how to take the pill. In trials, patients understood instructions 40% better. By 2025, over half of U.S. pharmacies plan to offer this.
But here’s the catch: not everyone has a smartphone. That’s why the basics still matter. Even with digital help, you still need to know how to read the paper label.
Why This Matters More Than You Think
Medication errors send over 1.5 million people to the ER every year in the U.S. The National Academies say two-thirds of those are preventable. And most of them? They start with a label that wasn’t read-or was misunderstood.People who understand their labels are 28% more likely to take their medicine correctly. That means fewer hospital visits, less pain, and lower costs. It also means your doctor can actually tell if the treatment is working-not if you forgot to take it.
And it’s not just about pills. It’s about control. When you understand your label, you’re not just following orders-you’re participating in your own care. That’s powerful.
Final Tip: Ask Before You Leave
Pharmacists don’t mind being asked. Seriously. They’ve seen it all. Walk up to the counter and say: “Can you go over this with me? I want to make sure I’m taking it right.”They’ll appreciate it. And you’ll sleep better knowing you didn’t guess.
What should I do if the pill looks different from my last prescription?
Don’t take it. Even if the label says it’s the same drug, the appearance might have changed due to a different manufacturer. Call the pharmacy and ask if they switched brands. If they did, ask if the dosage is the same. If you’re still unsure, ask for a consultation with the pharmacist. It’s better to wait than to risk taking the wrong thing.
What does “take with food” really mean?
It means eat something before or while you take the pill-not just a sip of water. A small snack like crackers, toast, or yogurt is enough. This helps your stomach absorb the medicine properly and prevents nausea or irritation. If you take it on an empty stomach, you might feel sick or the drug won’t work as well.
Can I split my pill if the label doesn’t say I can?
Only if it’s scored (has a line down the middle) and your doctor or pharmacist says it’s safe. Some pills have coatings or timed releases that get ruined if split. Splitting a pill that shouldn’t be split can change how much medicine you get-or make it dangerous. Always ask before cutting.
What if I miss a dose?
Check the label or call your pharmacy. If you miss a dose and it’s close to your next one (within 2 hours), skip it. Don’t double up. If it’s been longer than that, take it as soon as you remember. Never take two doses at once unless told to. For some drugs, like antibiotics, missing a dose can make them less effective.
Why do some labels say “discard after one year”?
The FDA doesn’t require expiration dates beyond one year for prescriptions, because most medications are used up before then. But after a year, the chemical makeup can change. The medicine might lose strength-or, in rare cases, break down into harmful substances. Even if it looks fine, don’t take it past that date. Dispose of it safely at a pharmacy drop-off.

14 Comments
This is literally the most important thing I've read all year. I used to just throw my pill bottles in a drawer and hope for the best. Now I check every label like it's a treasure map. Seriously, do this. Your future self will thank you.
PS: I printed this out and taped it to my medicine cabinet.
They say 'take with food' but never say what food. Like am I supposed to eat a steak or just a cracker? My pharmacist just shrugged. So I eat toast. Always toast.
I love how this post treats patients like capable humans instead of dumb kids who need a cartoon. Finally someone gets it. The fact that pharmacists are legally required to explain? That’s the golden rule right there. Use it.
I’ve been on five different meds in the last three years and each time I thought I understood the label until I got home and realized I had no idea what 'q.i.d.' meant or why my pill looked like a rainbow gummy bear. I started taking photos of every label the moment I got it. Now I have a whole folder called 'Pill Identification' on my phone. I also keep a little notebook next to my coffee maker with the times I take each one. It’s weirdly satisfying. Like a tiny ritual of self-preservation. And honestly? It’s made me feel less like a patient and more like a person who’s got this under control. I wish more people knew this stuff. Not because it’s hard-it’s not-but because no one ever taught us how to ask.
I scanned the QR code on my last prescription and it showed a 30-second video in Spanish of my abuela taking her pill with water. I cried. Not because I’m emotional (okay maybe a little) but because someone finally thought about people like my mom who don’t read English but still need to survive. This isn’t just info-it’s dignity.
took my med this morning like the label said and now i feel like a superhero. also i wrote the time on my hand with a sharpie. dont judge. it works.
Americans think labels are too complicated? Try dealing with a 12-page pamphlet in 5 languages and no one to translate. We need better systems not more reading. Stop making patients into pharmacists.
I’ve been teaching my elderly neighbors how to read their labels. One of them told me she used to take her blood pressure med at bedtime because it said 'take once daily' and she thought that meant 'when you go to sleep.' I sat with her for 20 minutes and drew a clock. She cried. Not from sadness-from relief. We don’t need more technology. We need someone to sit down and say: 'Let me show you.'
In India, we don’t have QR codes or printed labels with clear instructions. We have a pharmacist who yells over the counter while handing you a bag. But we also have families. We have mothers who sit with their children for hours explaining what each pill does. We don’t have perfect systems-but we have love. And sometimes, that’s the only label that matters.
It is a profound and undeniable truth that the current paradigm of pharmaceutical communication is fundamentally flawed, inadequately designed for the cognitive load of the average citizen, and indicative of a systemic failure to prioritize human comprehension over bureaucratic efficiency. One must question the very foundations of a system that assumes literacy, numeracy, and temporal awareness as baseline conditions for survival.
I mean… if you can’t read a label, maybe you shouldn’t be taking pills. It’s not that hard. Just look at the words. It’s not rocket science. People just don’t try.
Bro I just use my AI assistant to scan the label and it tells me everything in Hindi + English + emojis 😎💊🌅. Why are we still using paper? This is 2025. You guys are living in 1998. #SmartLife #PharmaTech
The real problem isn’t the label. It’s the fact that we let corporations design our medicine instructions. In ancient times, healers spoke directly to the patient. Now we get a barcode and a pamphlet written by a committee. We’ve lost the sacred connection between healer and human. This isn’t healthcare. It’s a transaction.
I work in a pharmacy. I’ve seen people take pills they were never prescribed. I’ve seen people mix alcohol with sedatives because they didn’t read the sticker. I’ve seen grandparents give their grandkids their meds because ‘they looked the same.’ This isn’t about intelligence. It’s about fatigue. People are tired. They’re overwhelmed. They’re scared. They just want to get better. If we want fewer errors, stop blaming them. Start designing for them.
Write a comment