Why Heat Turns Ordinary Medications Into Dangerous Risks for Seniors
When the temperature climbs, most people think about staying cool, drinking water, and avoiding the sun. But for seniors on certain medications, heat isn’t just uncomfortable-it can be life-threatening. The body’s ability to regulate temperature weakens with age, and many common prescriptions make that problem worse. Diuretics, blood pressure meds, antipsychotics, and even over-the-counter sleep aids can interfere with sweating, thirst, and fluid balance. The result? A silent, fast-moving risk of heat exhaustion or heat stroke that often goes unnoticed until it’s too late.
In 2023, the CDC reported that seniors taking two or more medications are 60% more likely to suffer heat-related emergencies than those on one or none. And with summer temperatures rising year after year, this isn’t a rare issue-it’s becoming a predictable danger. The good news? You can prevent most of these problems with simple, targeted steps.
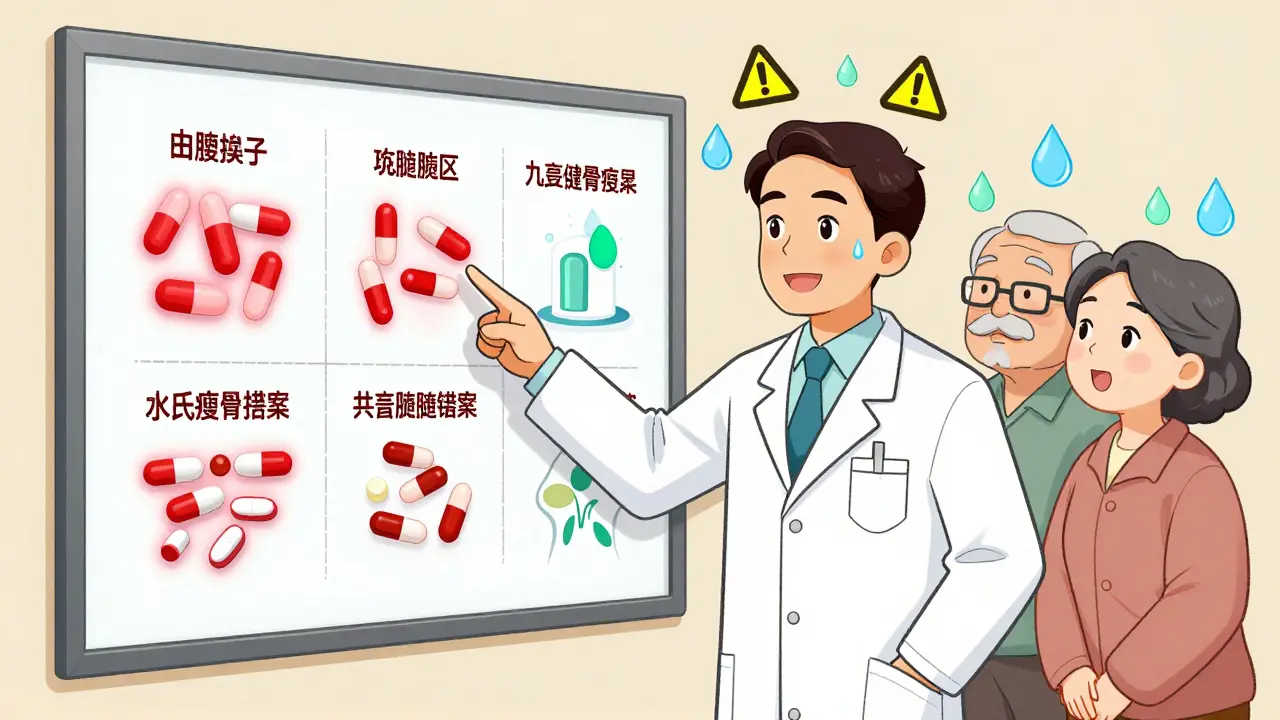
Medications That Turn Up the Heat Risk
Not all medications are equal when it comes to heat. Some are quietly sabotaging the body’s cooling system. Here are the top offenders:
- Diuretics (like hydrochlorothiazide and furosemide): These pills help reduce fluid buildup but also make you lose more water through urine. Studies show they reduce thirst by 30-40%, so seniors often don’t feel the need to drink-even when they’re dangerously dehydrated.
- ACE inhibitors and ARBs (like benazepril, losartan): Used for high blood pressure, these drugs can lower blood volume and reduce the urge to drink water. When combined with diuretics, the risk multiplies.
- Antipsychotics (like quetiapine, clozapine): Common in dementia care, these drugs disrupt the brain’s thermostat. Research shows they can raise core body temperature by 1.5-2.0°F even without physical activity.
- Anticholinergics (like diphenhydramine in Benadryl or Tylenol PM): These block sweat production by 35-50%. No sweat means no cooling. In hot weather, this can cause body temperature to spike dangerously fast.
- Certain antibiotics and antifungals: Some, like tetracycline or fluconazole, make skin far more sensitive to UV rays. Sunburn can happen in under 15 minutes, increasing dehydration and heat stress.
What makes this worse? Most seniors take multiple medications. A 2022 study found that 87% of adults over 65 are on two or more prescriptions. That means the effects stack up. A person on a diuretic, an ACE inhibitor, and an anticholinergic isn’t just at risk-they’re in a perfect storm.
What to Do Before Summer Hits
Waiting until it’s hot to think about this is too late. The best time to act is in early spring. Here’s what to do:
- Review every medication with a doctor or pharmacist. Bring a full list-prescriptions, supplements, and OTC drugs. Ask: “Does this make me more sensitive to heat?” Don’t assume your doctor knows all the interactions. Pharmacists are trained specifically for this.
- Ask about dose adjustments. For some seniors, lowering the dose of a diuretic on hot days can prevent dangerous dehydration. This isn’t something to guess at-work with your provider to create a heat-season plan.
- Check fluid restrictions. Many seniors with heart failure are told to limit fluids. But during heat waves, those restrictions can be deadly. Talk to your doctor about whether it’s safe to drink more on hot days.
- Replace risky OTC meds. If you take diphenhydramine for sleep or allergies, switch to a non-anticholinergic option like loratadine or melatonin. Ask your pharmacist for safer alternatives.
A 2022 study from Johns Hopkins showed that seniors who had a structured medication review before summer had 37% fewer heat-related ER visits. That’s not a small number-it’s life-saving.
Hydration That Actually Works
Drinking water isn’t enough if you’re on the wrong meds. Here’s how to hydrate properly:
- Drink 8-10 glasses of water daily during hot weather, even if you’re not thirsty. Your body won’t signal you properly.
- Avoid caffeine and alcohol. Both increase urine output by 40-60%. One coffee or glass of wine can undo hours of hydration.
- For those on diuretics, choose electrolyte drinks. Look for beverages with 120-150 mg of sodium per 8 oz. This helps replace what’s lost through urine without raising blood pressure.
- Don’t wait for thirst. Seniors on heat-risk meds often don’t feel thirsty until they’re already dehydrated. Set alarms to drink every 90 minutes.
Water alone won’t fix electrolyte imbalances. That’s why sports drinks or oral rehydration solutions (like Pedialyte) are better than plain water for many seniors on diuretics.
Stay Cool Without Relying on Luck
Heat doesn’t just come from the sun-it builds up indoors. Here’s how to keep your environment safe:
- Keep indoor temps below 78°F (25.6°C). If you don’t have air conditioning, go to a public library, mall, or community center during peak heat hours (10 a.m.-4 p.m.).
- Wear loose, light-colored cotton clothing. Synthetic fabrics trap heat. Cotton lets skin breathe and can lower perceived temperature by 5-7°F.
- Use sunscreen daily. If you’re on sun-sensitive meds, your skin burns 4-6 times faster. Use SPF 30 or higher, and reapply every 2 hours-even if it’s cloudy.
- Take cool showers or use damp cloths. Dampening your wrists, neck, and forehead helps cool blood flow. Don’t wait until you feel overheated-do it proactively.
One assisted living facility in Arizona cut heat-related incidents by 29% in 2022 just by moving residents indoors during the hottest part of the day and checking their temperature twice daily.
Recognizing the Warning Signs-Before It’s Too Late
Heat exhaustion doesn’t always look like the movies. Seniors often show subtle, confusing symptoms:
- Confusion or dizziness (even if they’re not standing)
- Reduced alertness or slurred speech
- Nausea or vomiting
- Muscle cramps
- Headache
- Dark urine or very little urine
Heat stroke is an emergency. Signs include:
- Body temperature above 103°F (39.4°C)
- Hot, dry, or damp skin (no sweating)
- Rapid, strong pulse
- Loss of consciousness
Here’s the hard truth: 41% of seniors on heat-risk meds don’t show classic symptoms. That’s why caregivers need to watch for changes in behavior-not just physical signs. If a normally alert senior seems unusually quiet, confused, or sluggish, treat it like a medical emergency.
According to UCLA research, caregivers who checked for these subtle changes reduced heat stroke progression by 62%. That’s not luck-it’s vigilance.
What to Do If Symptoms Appear
If you suspect heat exhaustion or heat stroke:
- Move to a cool place immediately-ideally air-conditioned.
- Remove excess clothing.
- Apply cool, wet cloths to the neck, armpits, and groin.
- Give cool fluids if the person is alert and able to swallow.
- Call 911 if: the person is confused, unconscious, has a body temperature above 103°F, or doesn’t improve within 30 minutes.
Don’t wait. Heat stroke can cause permanent brain or organ damage within hours. The CDC says 65% of heat exhaustion cases turn into heat stroke if untreated.

New Tools to Help You Stay Safe
In 2023, the CDC launched the Heat and Medication Risk Assessment Tool (HM-RAT). It lets you enter your medications and location to get a personalized heat risk score. The National Institute on Aging also partnered with the EPA to create HeatRisk.gov, which combines weather forecasts with medication risk data. Both are free and available online.
There’s also promising research underway. A new “heat resilience” supplement-designed for seniors on multiple meds-showed 28% better temperature control in early trials. While not yet widely available, it signals a growing focus on protecting vulnerable seniors from climate-related health threats.
Final Thought: Prevention Is a Team Effort
Preventing heat-related medication problems isn’t just about what the senior does-it’s about what family, caregivers, and doctors do together. A checklist, a daily check-in, a conversation with a pharmacist-these small actions add up. With climate change making extreme heat more common, these steps aren’t optional. They’re essential.
Can seniors stop taking their meds during hot weather?
No. Never stop or change a prescription without talking to a doctor. Some medications, like those for blood pressure or heart conditions, can be dangerous if stopped suddenly. Instead, ask your provider about adjusting the dose or timing during hot weather. Many can safely reduce diuretics or shift timing to earlier in the day to avoid nighttime dehydration.
Are over-the-counter painkillers safe in the heat?
Most NSAIDs like ibuprofen and naproxen are generally safe, but they can affect kidney function in seniors, especially when dehydrated. Acetaminophen (Tylenol) is usually a better choice for pain or fever during heat waves. Avoid combination products that include diphenhydramine, like Tylenol PM-it blocks sweating and increases heat risk.
Do I need to worry about heat if I stay indoors all day?
Yes. Indoor temperatures can rise 15-20°F above outdoor temps without air conditioning. A house with poor ventilation or dark curtains can become a heat trap. Seniors on heat-risk meds can develop heat exhaustion even while sitting on the couch. Keep windows shaded, use fans, and aim to keep indoor temps below 78°F.
What’s the best way to monitor a senior’s hydration?
Check urine color-pale yellow is good. Dark yellow or amber means dehydration. Also watch for dry mouth, low skin elasticity (pinch the back of the hand-if it doesn’t snap back quickly, they’re dehydrated), and confusion. Weighing the senior daily can help too-a 2-pound drop in a day signals fluid loss.
Can heat affect how medications work?
Yes. Heat can change how the body absorbs, breaks down, and eliminates drugs. For example, dehydration can make blood levels of certain meds rise dangerously high, increasing side effects. Some medications, like lithium for bipolar disorder, require close monitoring in heat because the margin between safe and toxic levels is very narrow. Always tell your doctor if you’ve been in hot weather.
Next Steps for Families and Caregivers
Start today. Print out a list of the senior’s medications. Go to HeatRisk.gov and enter their zip code and meds. Call their pharmacist and ask: “Which of these increase heat risk?” Schedule a doctor’s visit before summer. Make a plan: when to drink, where to go if it gets hot, what signs to watch for. Keep a thermometer in the home. Write down emergency contacts. These aren’t extra tasks-they’re the difference between a hot day and a medical crisis.

15 Comments
Hydration isn't optional. Set alarms. Drink water. No excuses.
Simple. Effective.
My grandma takes five meds and lives alone. I printed this out and taped it to her fridge. She doesn't read much but she reads the list. Changed everything.
In India we call this 'garam ka darr' - fear of heat. But here, nobody talks about meds. We fix the fan, not the pill bottle. This post? Needed.
I’ve been telling my aunt for years to swap Tylenol PM for melatonin. She said 'but it helps me sleep!'
Turns out it also helps her nearly pass out in July. Switched last month. No more ER trips. Thank you for the science.
Let’s be honest - most seniors on multiple meds are being managed by overworked primary care docs who haven’t read a pharmacology textbook since 2010. Pharmacists are the unsung heroes here. And yet, we still treat them like glorified cashiers. The system is broken. This isn’t just about hydration - it’s about systemic neglect disguised as medical care.
It is truly lamentable that we have reached a point where the elderly are being pharmacologically sedated into thermal vulnerability, as though their bodies were mere vessels to be managed by algorithmic prescriptions rather than biological organisms worthy of holistic consideration.
One cannot help but wonder if the pharmaceutical-industrial complex has, in its infinite wisdom, deemed heat stroke a manageable cost of doing business.
You missed the big one - SSRIs. They impair thermoregulation just as badly as anticholinergics. I work in geriatric psych. Every summer we have three to five cases of heat stroke in patients on sertraline or fluoxetine. No one talks about it because 'it's just depression meds.'
It's not just diuretics and Benadryl. It's everything.
So let me get this straight - we’ve got a national crisis where people are dying because their meds make them oblivious to thirst, and the solution is... more lists?
What a brilliant use of human ingenuity.
My dad’s on hydrochlorothiazide and losartan. We started giving him electrolyte packets at breakfast. He says he hasn’t felt so 'light' in years. No drama. Just hydration. You don’t need a PhD to do this.
Just told my mom to stop taking her night-time Benadryl. She cried. Said it was the only thing that helped her sleep.
Switched to 3mg melatonin + white noise. She’s sleeping better and not sweating through her pajamas at 3am. 🙌
This is what happens when you let people over 65 live in homes without central AC. The real issue isn’t the meds - it’s the collapse of infrastructure. If you can’t afford to cool your house, no list of pills will save you. Blame the politicians, not the pharmacists.
The data presented here is not merely suggestive - it is statistically robust, epidemiologically significant, and clinically actionable. The confluence of polypharmacy, age-related autonomic decline, and ambient thermal stress constitutes a quintessential public health triad. One must, therefore, advocate for structured medication reconciliation protocols, standardized heat-risk scoring integration into EHRs, and mandatory pharmacist-led patient education modules prior to seasonal temperature escalation. The CDC’s HM-RAT tool, while commendable, remains underutilized due to institutional inertia and a pervasive lack of interprofessional coordination.
I’m curious - has anyone looked at how heat affects the pharmacokinetics of anticoagulants? My uncle’s on warfarin and had a weird INR spike last summer. Doc blamed 'dehydration' but never said why. Is this documented?
We treat heat like a weather problem. But it’s a care problem.
People don’t die because it’s hot.
They die because no one checked on them.
Because we forgot that aging isn’t a disease to be managed - it’s a life to be held.
I work at a senior center. We started doing daily hydration checks - just asking 'did you drink anything today?' - and now we have zero heat-related incidents this summer. It’s not fancy. It’s just showing up.
Write a comment