When someone starts gender-affirming hormone therapy (GAHT), they’re not just changing their body-they’re starting a long-term medical journey. And like any long-term medication plan, what you take alongside your hormones matters. Gender-affirming hormone therapy can interact with other drugs in ways that either reduce effectiveness or raise risks. These aren’t theoretical concerns. Real people, real side effects, real changes in how their medications work.
How Hormones Work in the Body
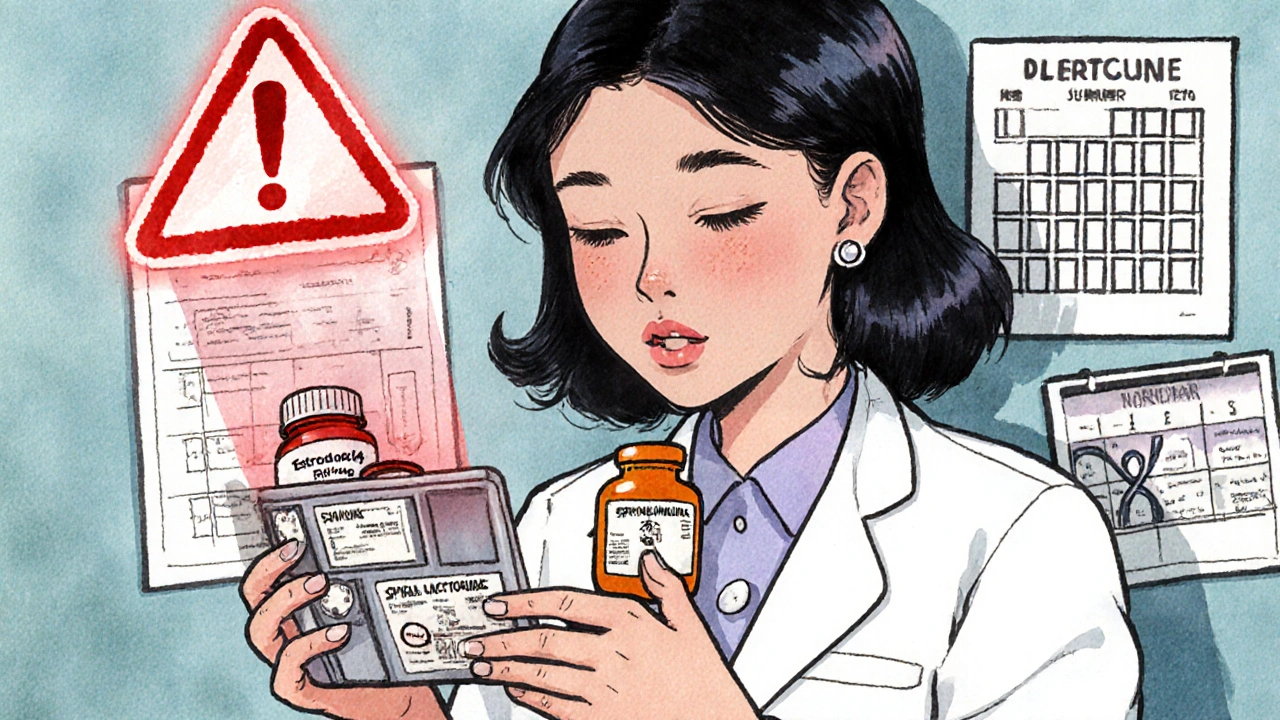
Feminizing hormone therapy usually means taking estradiol-often as a patch, pill, or injection-and an anti-androgen like spironolactone or cyproterone acetate. Masculinizing therapy means taking testosterone, usually as a gel, injection, or pellet. These aren’t simple chemicals. They’re processed by your liver, broken down by enzymes, and can interfere with or be interfered with by other drugs. The biggest player here is the CYP3A4 enzyme. It’s responsible for breaking down about half of all medications you take. Estradiol is mainly metabolized through this pathway. That means anything that boosts or blocks CYP3A4 can change how much estradiol stays in your system. Testosterone, on the other hand, gets converted by enzymes like 5-alpha reductase and aromatase. These are less commonly affected by other drugs, which is why testosterone interactions are fewer and less dramatic.Antiretrovirals and HIV Medications: A High-Stakes Mix
Transgender women are 40 times more likely to be living with HIV than cisgender women. That means many people on feminizing hormones are also taking antiretroviral therapy (ART). And here’s where things get tricky. Some HIV drugs, like efavirenz and rifampin, speed up CYP3A4. That means they can drop estradiol levels by 30-50%. If you’re on one of these, you might start feeling like your hormones aren’t working anymore-less breast development, mood swings, or fatigue. Your provider may need to bump up your estradiol dose. On the flip side, drugs like cobicistat (used in combo pills like Stribild or Descovy) block CYP3A4. That can cause estradiol to build up-sometimes by 40-60%. That raises the risk of blood clots, high blood pressure, or liver stress. One study found estradiol levels spiked within two weeks of starting cobicistat. Monitoring hormone levels after switching ART is not optional-it’s essential. Good news? Integrase inhibitors like dolutegravir don’t interfere with estradiol. They’re the safest choice if you’re starting both HIV treatment and GAHT at the same time.PrEP: Safe to Use With Hormones
If you’re on PrEP to prevent HIV, you’re probably taking tenofovir disoproxil fumarate and emtricitabine (TDF/FTC). A 2022 study of 172 transgender people on PrEP and GAHT found no meaningful changes in hormone levels or PrEP effectiveness. Estradiol didn’t affect how well tenofovir worked. Testosterone didn’t change how the body processed the PrEP drugs. Levels stayed within safe, protective ranges. This is one of the clearest, most reassuring findings in recent years. You can safely take PrEP with GAHT. No dose adjustments needed. Just keep getting tested every three months, as recommended.
Psychiatric Medications: The Hidden Risk
Transgender people experience depression, anxiety, and PTSD at rates two to three times higher than the general population. Many are on SSRIs like fluoxetine or sertraline. But here’s the gap: almost no clinical trials for antidepressants include transgender participants. Some SSRIs, especially fluoxetine and paroxetine, can slow down CYP2D6, another liver enzyme. That can slightly raise estradiol levels. Not enough to be dangerous, but enough to cause unexpected side effects-like breast tenderness or mood shifts-if you’re already on the higher end of your hormone dose. Bigger concern: carbamazepine, phenytoin, and rifampin (used for seizures or TB) are strong CYP3A4 inducers. They can make estradiol less effective. One case report described a transgender woman who lost breast development after starting carbamazepine. Her estradiol levels dropped by 60%. Her dose had to be doubled. Testosterone doesn’t seem to interfere with most antidepressants. But a 2023 review found 17 cases where people on testosterone needed higher doses of their antidepressants within six weeks of starting hormones. Why? Possibly because testosterone changes brain chemistry in ways that affect serotonin. If your mood suddenly worsens after starting testosterone, don’t assume it’s just adjustment. Talk to your provider about checking your antidepressant levels.Other Common Medications to Watch
- Birth control pills: These contain estrogen. If you’re already on feminizing hormones, adding another estrogen source can raise your risk of blood clots. Stop oral contraceptives before starting GAHT. - Statins (like atorvastatin): These are broken down by CYP3A4. High estradiol levels may increase statin concentration, raising the risk of muscle damage. Monitor for unexplained muscle pain. - Thyroid medication: Estradiol increases thyroid-binding proteins. That can make your free T4 levels look low on blood tests-even if you’re not hypothyroid. Your doctor may need to adjust your levothyroxine dose based on symptoms, not just lab numbers. - Antibiotics: Most are fine. But rifampin is a strong CYP3A4 inducer. If you’re on it for TB, expect your estradiol to become less effective. Plan ahead.What About GnRH Agonists?
GnRH agonists like leuprolide are used to pause puberty in teens or suppress natural hormones in adults. The good news? They don’t interact with any HIV meds, antidepressants, or common prescriptions. They’re metabolized differently-through the kidneys, not the liver. That makes them one of the safest options when you’re on multiple medications. But they’re expensive. And they can cause bone density loss if used long-term without calcium or vitamin D. Always pair them with monitoring.
What Should You Do?
1. Make a full list of every medication, supplement, and over-the-counter drug you take-including CBD, St. John’s Wort, and herbal teas. 2. Bring it to every appointment. Don’t assume your provider knows what you’re on. Many clinics still don’t have standardized screening tools. 3. Ask for hormone level checks after starting or changing any new medication. Estradiol and testosterone levels should be checked 4-6 weeks after a drug change. 4. Don’t stop or change doses on your own. Even if you feel fine, a small change in metabolism can have big consequences over time. 5. Use a pharmacist. Many pharmacies now have pharmacists trained in transgender health. They can flag interactions you might miss.What’s Changing in 2025?
The NIH is running the Tangerine Study, tracking how 300 transgender adults respond to 12 common psychiatric drugs alongside GAHT. Results are expected in mid-2025. That’s the first large-scale data we’ll have on antidepressants and hormones. The FDA is now pushing drugmakers to include transgender people in clinical trials. Gilead, the maker of Truvada and Descovy, now requires GAHT interaction data for all new PrEP studies. That’s a big shift. But gaps remain. We still don’t know how cabotegravir (the long-acting PrEP shot) interacts with hormones. Or how newer antidepressants like brexanolone affect testosterone levels. We’re learning fast-but we’re not done.Bottom Line
Gender-affirming hormone therapy is safe. But safety doesn’t mean ignoring other meds. The real risk isn’t the hormones themselves-it’s the blind spots in care. Many providers still don’t know how GAHT interacts with HIV drugs, antidepressants, or even common antibiotics. Your best defense? Be informed. Keep track. Ask questions. And never assume something is safe just because no one’s talked about it yet.Can I take birth control while on gender-affirming hormones?
No. Birth control pills contain estrogen, which adds to your hormone load and increases the risk of blood clots, stroke, and high blood pressure. If you’re on feminizing hormone therapy, stop oral contraceptives. Use non-hormonal methods like condoms, copper IUDs, or sterilization instead.
Do antidepressants stop hormones from working?
Not usually. But some antidepressants like fluoxetine can slightly raise estradiol levels by blocking liver enzymes. On the other hand, if you start testosterone and your depression gets worse, your antidepressant may need a higher dose. Hormones change brain chemistry-your mental health meds might need adjusting too.
Is it safe to take PrEP with testosterone or estradiol?
Yes. A 2022 study of 172 transgender people found no meaningful changes in hormone levels or PrEP effectiveness when taken together. Tenofovir levels stayed within protective ranges. You can safely use PrEP with GAHT without dose changes.
What should I do if I start a new antibiotic?
Most antibiotics are fine. But avoid rifampin-it’s a strong enzyme inducer that can cut estradiol levels in half. If you’re prescribed rifampin for TB, tell your endocrinologist right away. You may need a higher hormone dose. For other antibiotics, no action is needed.
How often should I get my hormone levels checked when starting a new medication?
Four to six weeks after starting or changing any new drug-especially HIV meds, antidepressants, or seizure medications. That’s when enzyme changes show up in your blood. After that, check every 3-6 months if you’re stable. If you feel off-fatigue, mood changes, less hormone effects-get tested sooner.

15 Comments
Man, I’ve been on estradiol for five years now, and the first time my HIV med switched to cobicistat, I thought I was going insane. Mood swings like a damn rollercoaster, breasts feeling like they were swelling overnight, and then my doc pulls up my labs-estradiol up 58%. I almost got scared off hormones altogether. But here’s the thing: it’s not magic, it’s biochemistry. Your liver doesn’t care about your identity, it just does its job. If you’re on ART, get your levels checked every time your meds change. No excuses. This isn’t just about gender-it’s about survival.
And yeah, I know some folks think ‘hormones are just hormones,’ but if you’re stacking them with antivirals, antidepressants, even damn turmeric supplements, you’re playing Russian roulette with your liver. I’ve seen people crash. I’ve seen people thrive. The difference? Documentation. Communication. And not being too proud to ask a pharmacist for help.
Also-stop taking St. John’s Wort. I don’t care if it’s ‘natural.’ It’s a CYP3A4 inducer. It’ll make your estrogen useless. And no, your yoga instructor doesn’t know more about pharmacokinetics than your endocrinologist.
TL;DR: Know your meds. Track your labs. Don’t trust Google. And for the love of god, tell your provider everything-even the herbal tea you drink at 2 a.m.
So let me get this straight-you’re telling me a transgender woman on PrEP and estradiol can’t get HIV, but if she takes rifampin for TB, her hormones turn to dust? And we’re still acting like this is normal? This isn’t medicine. This is a glitch in the system. Someone designed a hormone therapy that breaks when you’re sick. Someone designed an HIV drug that overloads estrogen. And we’re just supposed to ‘adjust’? Like it’s a damn video game difficulty setting?
Meanwhile, cis guys take statins, antidepressants, and antibiotics without a single lab test. But if you’re trans? Better bring your spreadsheet, your bloodwork, your pharmacy receipt, and your therapist’s note. This isn’t healthcare. It’s performance art with a side of bureaucracy.
This is a very important article. In India, many transgender individuals begin hormone therapy without medical supervision due to lack of access. The interactions described here are not just theoretical-they are life-threatening. I urge all healthcare providers to learn about GAHT interactions, and for patients to seek care even if it is difficult. Your health matters. Please do not delay. Also, if you are using herbal remedies like ashwagandha or turmeric, speak to your doctor-they may interfere with hormone metabolism. Safety first.
Everyone’s acting like this is new info. It’s not. The CYP3A4 interaction with estradiol has been documented since at least 2012. The fact that clinics are still surprised by this says more about how poorly trans healthcare is integrated into mainstream medicine than it does about the science. Also, ‘don’t stop meds on your own’-duh. But if your provider doesn’t know this stuff, who’s supposed to? The pharmacist? The Reddit thread? We need standardized protocols, not scattered case reports.
It is imperative that individuals undergoing gender-affirming hormone therapy maintain comprehensive medication reconciliation with their clinical team. The pharmacokinetic interactions outlined in this post are well-supported by peer-reviewed literature, including studies published in The Journal of Clinical Endocrinology & Metabolism and AIDS Patient Care and STDs. Failure to monitor estradiol concentrations following initiation of CYP3A4 modulators may result in clinically significant adverse events, including venous thromboembolism and hepatotoxicity. All patients should be advised to obtain baseline and follow-up hormone levels at four to six weeks post-intervention. Furthermore, the use of non-hormonal contraceptive methods is strongly recommended in conjunction with feminizing hormone regimens. Professional guidelines from WPATH and Endocrine Society support these recommendations.
It’s fascinating how medicine treats gender as a variable to be controlled, rather than a lived experience. We reduce bodies to enzyme pathways, reduce identity to metabolic profiles. Is this what liberation looks like? A carefully calibrated drug regimen that requires you to be a pharmacology student just to survive? Maybe the real problem isn’t the interactions-it’s the system that forces us to navigate them in the first place.
Oh wow, so now we’re pretending that testosterone doesn’t interact with anything? Please. Everyone knows testosterone makes SSRIs less effective because it lowers serotonin receptors. And don’t even get me started on how estrogen makes men ‘emotional’-that’s not a side effect, that’s a feature. Also, why is everyone acting like PrEP is safe? What about the fact that tenofovir can cause kidney toxicity over time? And you’re telling me it’s fine to stack that with hormones? That’s not safety-that’s negligence. Someone’s gotta say it.
So… just don’t take any other meds then? Easy fix.
I’ve been on testosterone for eight years. I’ve had every single one of these interactions. I’ve had my antidepressants fail. I’ve had my liver enzymes spike. I’ve had my thyroid levels look fake because estrogen was hiding behind binding proteins. And here’s the truth no one says: the system doesn’t care if you live or die. They’ll give you a pamphlet and send you on your way. I’ve sat in waiting rooms for six months just to get a hormone level checked after starting a new antibiotic. No one taught me this. No one warned me. I learned it by almost dying. So now I tell everyone: if you’re on hormones, you’re not just a patient-you’re a detective. And if your doctor doesn’t know this stuff, find someone who does. Because you’re not going to survive this system by being polite.
For anyone new to this-don’t panic. This is manageable. I’ve mentored over 30 trans folks through GAHT and drug interactions. The key is simple: make a list. Every pill, every supplement, every tea. Take it to your endo and your pharmacist. Ask: ‘Will this change how my hormones work?’ Most pharmacists now have trans health training. If yours doesn’t, ask for someone who does. And if your doctor says ‘I don’t know,’ say ‘Okay, let’s get you a consult.’ This isn’t about being difficult-it’s about being smart. You deserve care that doesn’t put you at risk. You’re not a lab rat. You’re a person.
Stop being passive. If you’re on hormones and you start a new med, you don’t wait for your doctor to notice. You call your pharmacy. You check Lexicomp. You Google the interaction yourself. If your provider doesn’t know this stuff, they’re not qualified to be your endo. Period. You don’t owe them patience. You owe yourself survival. And if you’re too scared to ask questions, you’re letting them win. Get loud. Get specific. Bring printed studies. They’re not your friend if they don’t know the difference between CYP3A4 and CYP2D6.
I am from India, and I started hormones last year. I didn't know about any of this. I took vitamin D, ashwagandha, and birth control pills together because I thought they were all ‘good for me.’ I felt dizzy, my chest hurt, and my mood changed. I didn’t know why. This article saved me. I went to a clinic in Delhi that specializes in trans care, and they helped me stop the wrong things. I am now on estradiol only, with no supplements. I am learning slowly. Thank you for writing this. I will share it with my community.
Let’s be real-this whole thing is a cover. Big Pharma and the medical-industrial complex are using ‘drug interactions’ to scare trans people into lifelong dependency. Estradiol doesn’t need all these labs. Testosterone isn’t dangerous. They just want you hooked on monthly blood draws and $300 prescriptions. They don’t want you to know that sunlight, exercise, and a plant-based diet can regulate your hormones naturally. And why do you think they’re pushing ‘monitoring’? So they can bill you more. The ‘CYP3A4 enzyme’? That’s just a buzzword to make you feel stupid. I’ve been off all meds for two years. My gender is more real now than ever. Don’t let them sell you fear disguised as science.
Love this breakdown. I’m an Irish pharmacist and we’ve been training our staff on GAHT interactions since 2022. The biggest win? When a trans patient walks in with a list of meds and says, ‘I think this antibiotic might mess with my hormones’-and they’re right. That’s empowerment. We don’t just dispense pills anymore. We have conversations. I’ve had patients come back months later saying, ‘I stopped that herbal tea and my mood stabilized.’ That’s the stuff that matters. Keep sharing this. We need more of this in primary care.
One thing no one mentions: GnRH agonists are the unsung heroes here. If you’re on long-term meds and you’re worried about interactions, ask about leuprolide. It’s not perfect-it’s expensive, and it can mess with bone density-but it doesn’t touch your liver enzymes. That means you can stack it with HIV meds, antidepressants, even statins without a single interaction. It’s not the ‘sexy’ option, but if you’re on a complex med regimen, it’s the safest path forward. Talk to your doctor about it. It might be the missing piece.
Write a comment