What an ECG Test Really Shows
When your doctor orders an ECG, they’re not just checking if your heart is beating. They’re looking at the electrical signals that make it beat. Think of your heart like a house with wiring-each pulse of electricity tells a story. The ECG picks up those signals through small stickers (electrodes) placed on your chest, arms, and legs. Within minutes, it draws a graph showing how your heart’s rhythm flows. Is it steady? Too fast? Too slow? Are there gaps in the signal? These patterns can tell if you’ve had a silent heart attack, if your heart muscle is thickened, or if your heart’s electrical system is misfiring.
It’s not a perfect tool. A normal ECG doesn’t mean your heart is healthy. Many people with blocked arteries have perfectly normal resting ECGs. That’s why doctors don’t rely on it alone. But when you’re having chest pain or your heart feels off, an ECG is the fastest, safest first step. It’s painless, takes less than five minutes, and gives immediate clues. In fact, over 80% of emergency rooms use it as their first cardiac test for chest pain.
Why You Might Need a Stress Test
Some heart problems only show up when your heart is working hard. That’s where a stress test comes in. It forces your heart to pump harder-either by making you walk on a treadmill or by using medicine to mimic exercise. If a coronary artery is narrowed, your heart won’t get enough blood during exertion. That’s when the ECG picks up changes: the lines on the graph start to flatten or dip. That dip, called ST-segment depression, is one of the clearest signs of reduced blood flow.
Stress tests aren’t just for people with symptoms. If you’re over 50, have high blood pressure, diabetes, or a family history of heart disease, your doctor might suggest one-even if you feel fine. The goal isn’t to scare you. It’s to catch problems early. A 2022 study found that people who could walk 10 minutes on a treadmill during a stress test had a 50% lower risk of a major heart event over the next five years than those who couldn’t make it past five minutes.
Exercise vs. Chemical Stress Tests
Not everyone can run on a treadmill. Maybe you have arthritis, lung disease, or just can’t get your heart rate up. That’s when doctors turn to chemical stress tests. Instead of walking, you get medicine through an IV. Drugs like adenosine or dobutamine make your heart beat faster and harder, just like exercise. You might feel flushed, short of breath, or get a weird chest pressure. It sounds scary, but it’s normal. The effects last less than a minute and fade fast.
Exercise tests are preferred when possible. They give more real-world data-how long you lasted, how your blood pressure responded, how you felt. Chemical tests are more controlled, but they don’t show your actual fitness level. Both use the same ECG machine to monitor your heart. The biggest difference? Time. A treadmill test takes 10 to 15 minutes. A chemical test can take up to an hour because you have to wait for the drug to work and wear off.

What Happens During a Stress Test
You’ll wear comfortable clothes and shoes. No caffeine for 24 hours before-you can’t have coffee, tea, chocolate, or energy drinks. They interfere with the medicine used in chemical tests. You’ll have electrodes stuck to your skin and a blood pressure cuff on your arm. The test starts slow. On the treadmill, you’ll walk at 1.7 miles per hour with a 10% incline. Every three minutes, it gets harder-faster and steeper. Your doctor watches you like a hawk. If you feel dizzy, short of breath, or have chest pain, you say so. They’ll stop right away.
They’re not just watching the ECG. They’re watching you. Are you pale? Sweating too much? Is your breathing ragged? Your heart rate target is 85% of your maximum, which is roughly 220 minus your age. So if you’re 60, they’re looking for a heart rate around 136. If you reach that without symptoms and your ECG looks good, you’re done. If not, they’ll stop early and still get useful info.
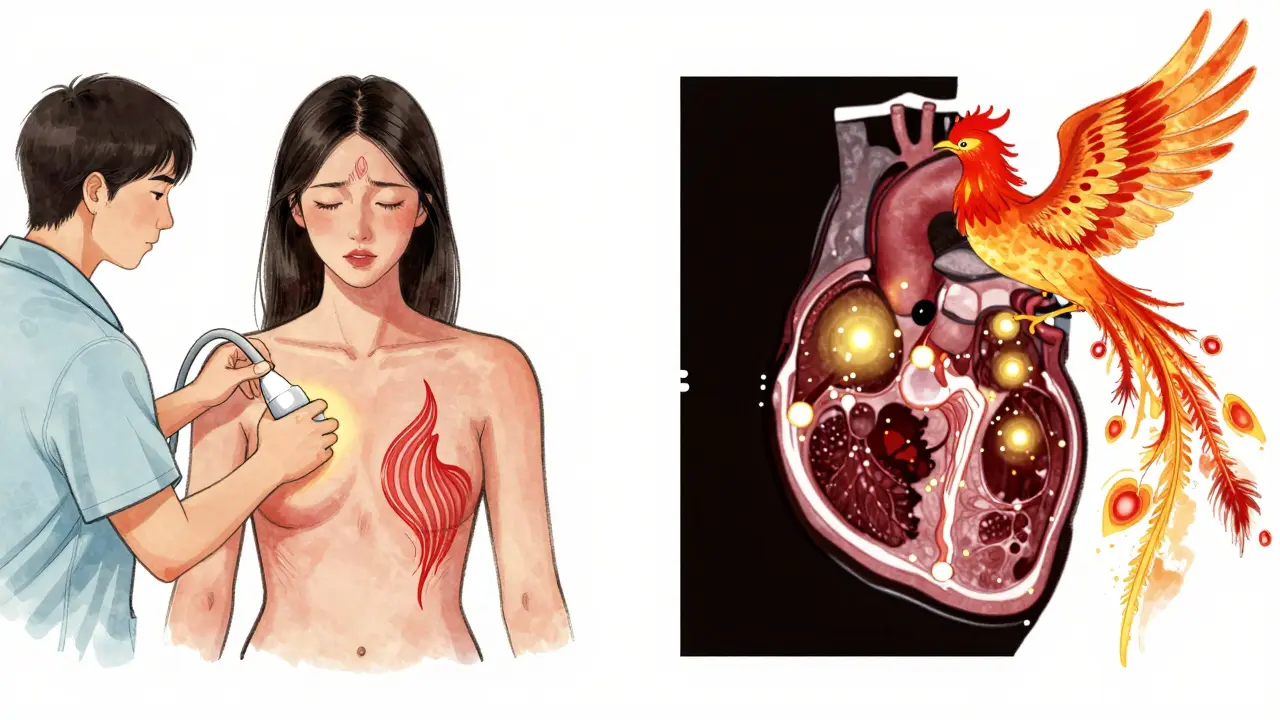
Stress Echo vs. Nuclear Stress Test
There’s more than one kind of stress test. The basic one uses just an ECG. But if your doctor wants to see how your heart muscle is moving, they’ll use stress echocardiography. That’s an ultrasound machine that takes pictures of your heart before and after stress. If a part of the heart doesn’t move well after exercise, it likely means that area isn’t getting enough blood. This test has higher accuracy than plain ECG stress testing-especially for women.
Nuclear stress tests use a tiny bit of radioactive dye. It travels through your bloodstream and lights up areas of your heart on a special camera. Healthy areas glow bright. Damaged or blocked areas stay dark. It’s more sensitive than echo-catches more blockages-but you’re exposed to radiation. A single test equals about three years of natural background radiation. It’s not dangerous, but doctors avoid it unless needed. For most people, stress echo is the better choice: no radiation, clearer pictures of heart motion, and just as accurate for detecting blockages.
What the Results Mean
Results aren’t just ‘normal’ or ‘abnormal.’ They’re graded. A test can be negative (no signs of disease), positive (clear signs of reduced blood flow), or inconclusive (something unclear). Inconclusive results happen in about 1 in 4 people, especially women and those with obesity or old ECG changes. If your test is inconclusive, you might need a stress echo, a CT scan, or even a cardiac catheterization.
Positive results don’t always mean you need surgery. A small blockage might just need lifestyle changes and medicine. But if your heart can’t handle even light exercise, or if multiple areas aren’t getting blood, your doctor will likely recommend further testing. The key is not the test result alone-it’s how it fits with your symptoms, risk factors, and overall health.
What You Should Know Before the Test
Prepare like you’re going for a workout. Wear loose clothes and walking shoes. Don’t eat a heavy meal two hours before. If you take heart meds like beta-blockers, ask your doctor if you should skip them-some interfere with the test. You’ll be asked to sign a consent form. That’s normal. The test is safe, but there’s a small risk of irregular heartbeat or chest pain. Staff are trained to handle it.
Many people worry about the results. That’s normal. But remember: this test isn’t a death sentence. It’s a tool. One woman in Portland told me her stress test caught a blockage she didn’t know she had. She changed her diet, started walking daily, and took medicine. Five years later, she’s hiking in the Columbia Gorge. That’s the point: catch it early, act on it, and live well.
Limitations and Who Should Avoid These Tests
ECG and stress tests aren’t perfect. They miss some problems-especially in women. Studies show up to 30% of women with heart disease get false-negative results on standard stress tests. Why? Their blockages are often in smaller vessels, not the big arteries. That’s why stress echo is now recommended for women with symptoms and intermediate risk.
Some people shouldn’t have stress tests at all. If you’ve had a heart attack in the last two days, have unstable chest pain, or have a severe heart rhythm problem, the test could be dangerous. If you’re extremely weak from illness or have aortic stenosis, your doctor will pick another path.
Also, don’t expect a stress test to show everything. It won’t detect early plaque buildup before it blocks blood flow. That’s where CT scans come in. But for most people, stress testing is the best balance of safety, cost, and usefulness.
What’s Next for Heart Testing
Technology is changing fast. New AI tools can now read ECGs faster and more accurately than most doctors. One study showed AI improved detection of hidden heart disease by nearly 20%. Portable devices like the Cardiac Dynamics StressPal let you do stress tests in your doctor’s office, at home, or even in a nursing home. That’s huge for older adults who can’t travel far.
Research is also focusing on women’s heart health. New techniques like speckle-tracking echocardiography can spot tiny changes in heart muscle movement that older tests miss. These tools are catching microvascular disease-the kind that affects women more often and was previously called ‘heart anxiety.’ Now we know it’s real. And we’re learning how to treat it.
Stress tests aren’t going away anytime soon. They’re affordable, widely available, and proven. But they’re becoming smarter, safer, and more personalized. The future isn’t about doing more tests-it’s about doing the right test, for the right person, at the right time.

9 Comments
I had my first ECG after fainting at work and thought I was dying. Turned out it was just anxiety and low iron. But wow, seeing that graph made it real. I still check my heart rate sometimes just to see if it looks "normal". Weird habit, I know.
My grandma did a chemical stress test last year and said it felt like her chest was being squeezed by a giant hand. She was fine after 30 seconds but honestly? I’m never getting one unless I have to.
Just wanted to say if you’re reading this and you’re scared about getting tested-don’t be. I was terrified too. I’m 58, diabetic, and my stress echo showed a tiny blockage. I started walking 30 minutes a day, cut out soda, and took my meds. Two years later? I hiked 12 miles in the Smokies with my grandkids. It’s not about the test. It’s about what you do after. You got this.
In India, most people think heart problems are only for old men. My mom had chest pain for months and no one believed her. Finally got a stress echo and found microvascular disease. No one talks about this. Women’s hearts are different. We need more awareness.
The part about AI reading ECGs better than doctors? That’s wild. I work in med tech and we’re already testing this in rural clinics. One device can flag a silent MI before the patient even knows something’s wrong. This isn’t sci-fi anymore.
i got my stress test last month and the doc said my ekg looked "weird" but i was fine. turns out i was just nervous and hyperventilating. still kinda mad they made me pay 500 bucks for that. also why no coffee? i need my morning brew
The clinical utility of stress testing lies in its ability to provoke ischemia under controlled conditions, thereby revealing functional deficits masked at rest. While resting ECGs have high specificity, their sensitivity for coronary artery disease is suboptimal, particularly in the context of balanced ischemia or microvascular dysfunction. Stress echocardiography improves diagnostic accuracy by integrating wall motion analysis with hemodynamic response-this is critical in populations with indeterminate ECG findings, such as women with left bundle branch block or baseline ST-T abnormalities. The shift toward non-invasive, radiation-free modalities reflects a paradigm evolution in preventive cardiology.
As someone who’s worked in cardiology for 22 years, I’ve seen the evolution from paper tracings to AI-enhanced ECGs. The biggest mistake? Assuming a normal resting ECG means no risk. We’ve missed too many women because we didn’t look beyond the big arteries. Stress echo isn’t just better-it’s fairer. And yes, the radiation from nuclear tests is low, but we still need to justify every exposure. Less is more when you’re doing it right.
The real breakthrough isn’t the tech-it’s the mindset shift. For decades, heart disease was seen as a man’s problem. We ignored microvascular angina, dismissed chest pressure as "anxiety," and told women to relax. Now we’re seeing that the heart’s smallest vessels can fail just as catastrophically as the big ones. Speckle-tracking echocardiography doesn’t just detect dysfunction-it validates the lived experience of thousands of women who were told they were imagining it. That’s not medicine. That’s justice.
Write a comment