Most people with diabetes don’t realize their eyes are quietly being damaged-until it’s too late. Diabetic retinopathy doesn’t come with warning signs like pain or sudden blur. It sneaks in, silently weakening blood vessels in the retina, the light-sensitive layer at the back of your eye. By the time you notice floaters, blurred vision, or dark spots, the damage is often advanced. But here’s the truth: diabetic retinopathy is preventable. With regular screening and timely treatment, 95% of vision loss from this condition can be avoided.
How Diabetes Turns Your Retina Into a War Zone
Your retina works like a camera sensor, turning light into signals your brain understands. But when blood sugar stays high for years, it starts corroding the tiny blood vessels that feed it. These vessels get weak, leak fluid, or block off completely. The eye tries to fix this by growing new blood vessels-but they’re fragile, messy, and useless. They bleed easily, scar the retina, and can even pull it loose from the back of the eye. This isn’t just a theory. It’s what happens in over 1 in 3 adults with diabetes in the U.S. According to the National Eye Institute, diabetic retinopathy is the leading cause of vision loss in people aged 21 to 64. That’s working-age adults-parents, teachers, nurses, truck drivers. Not just older folks. The longer you have diabetes, the higher your risk. Someone with diabetes for 20 years has nearly a 90% chance of some level of retinal damage. The real danger? You won’t feel it. No pain. No redness. No sudden blackout. That’s why so many people wait until they can’t read the clock or drive at night. By then, the retina has already suffered irreversible harm. Studies show 68% of patients only notice symptoms when the damage is already moderate or severe.The Three Stages of Retinal Damage
Diabetic retinopathy doesn’t jump from zero to blindness. It creeps forward in three clear stages:- Mild Nonproliferative Retinopathy: Tiny bulges, called microaneurysms, form in the blood vessels. These are like weak spots in a garden hose. They might leak a little fluid, but vision is still normal.
- Moderate to Severe Nonproliferative Retinopathy: More vessels get blocked. The retina starts to swell, especially in the macula-the center part responsible for sharp, detailed vision. This swelling is called diabetic macular edema (DME), and it’s what causes blurry, wavy vision. About 1 in 15 people with diabetes develop DME.
- Proliferative Diabetic Retinopathy: The retina, starved of oxygen, starts growing new blood vessels on its surface. These vessels are like paper-thin threads. They bleed into the vitreous (the gel inside your eye), causing sudden floaters or even total vision loss. They can also scar and pull the retina away from the eye wall, leading to detachment.
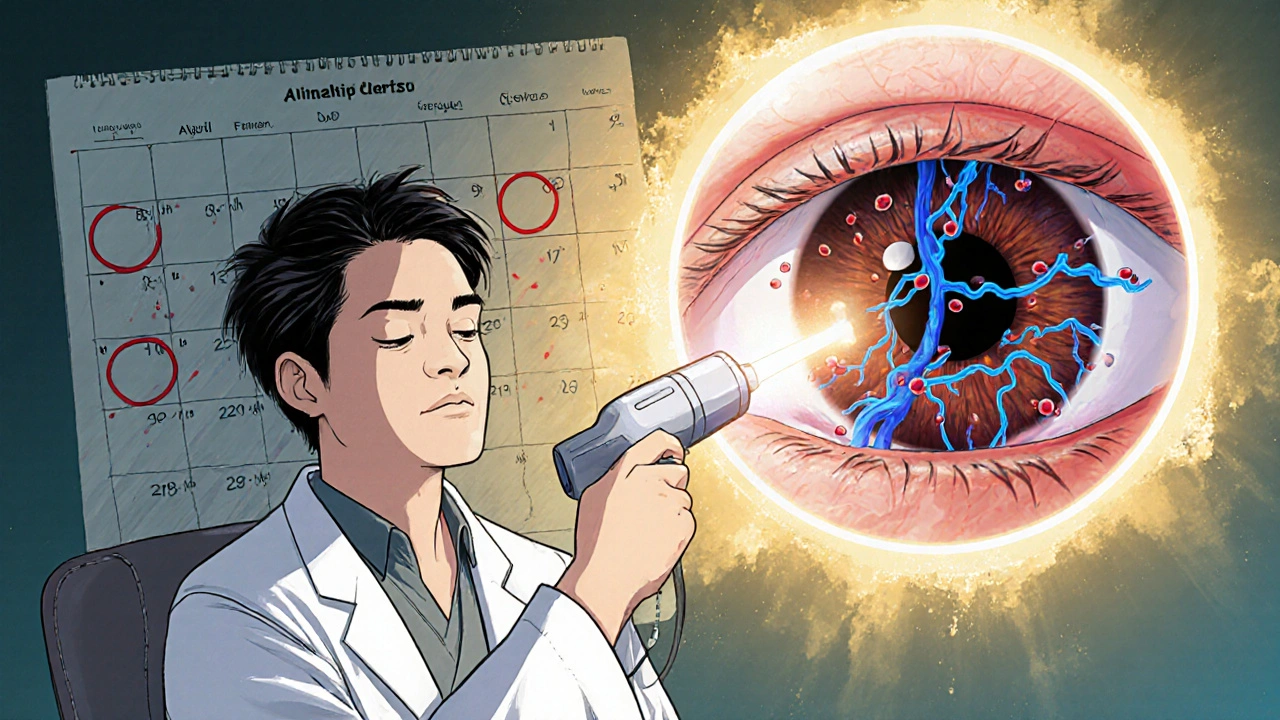
Why Laser Treatment Still Matters
For decades, laser therapy has been the go-to treatment for advanced diabetic retinopathy. It’s not glamorous. It’s not a pill. But it works. There are two main types of laser treatments:- Focal/Grid Laser Photocoagulation: Used for diabetic macular edema. The laser seals off leaking blood vessels in the macula. It doesn’t restore lost vision, but it stops further blurring. Studies show it reduces the risk of moderate vision loss by about 50%.
- Panretinal Photocoagulation (PRP): Used for proliferative retinopathy. The laser creates hundreds of tiny burns across the peripheral retina. This doesn’t help your side vision-but it tells the eye to stop growing those dangerous new blood vessels. It cuts the risk of severe vision loss by more than 50%.
What Happens If You Skip Treatment?
Ignoring diabetic retinopathy doesn’t mean you’ll just get blurry vision. It means you risk:- Vitreous hemorrhage: A sudden flood of blood into the eye. Vision goes from cloudy to completely dark.
- Retinal detachment: The retina peels away from the back of the eye. This is a medical emergency. Without surgery within days, blindness is likely.
- Neovascular glaucoma: New blood vessels grow over the eye’s drainage system. Pressure builds up, crushing the optic nerve. This type of glaucoma is extremely hard to treat and often leads to permanent blindness.
The Real Key: Control Your Blood Sugar
Laser treatment saves sight-but it doesn’t stop the damage from continuing. The only way to truly protect your eyes is to control your blood sugar. And not just a little. Consistently. Research from the Cleveland Clinic shows that keeping your A1C below 7% slows retinopathy progression by up to 76%. That’s not a suggestion. That’s science. High blood pressure and high cholesterol make it worse. Smoking? It doubles your risk. Think of it this way: laser treatment is like patching a leaky roof. But if you keep pouring water on it, the whole house will collapse. Managing diabetes is about stopping the rain.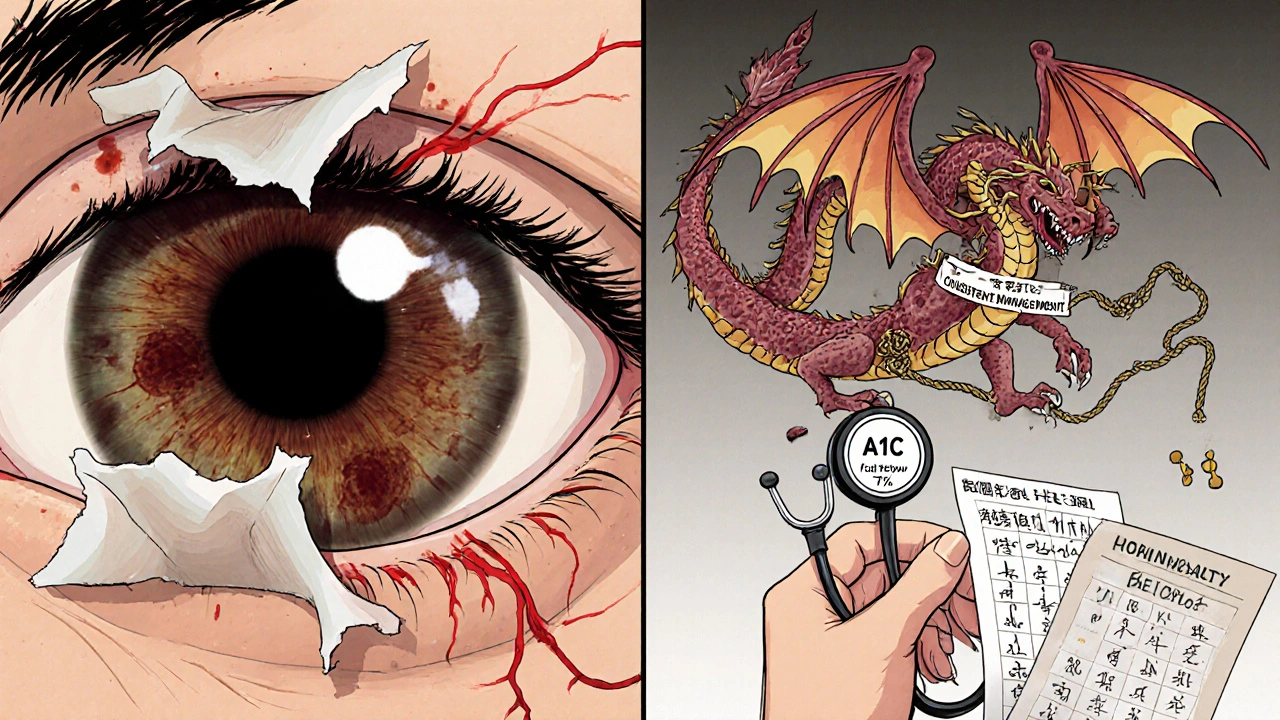
Screening: The Only Way to Catch It Early
If you have diabetes, you need a dilated eye exam every year. No exceptions. Even if your vision feels perfect. Even if you’ve had normal exams before. The American Diabetes Association and the NHS both recommend annual screenings for all adults with diabetes. For some-like pregnant women with diabetes or those already showing early signs-doctors may recommend exams every 3 to 6 months. During the exam, your eye doctor will use drops to widen your pupils. Then they’ll look at the retina with a special magnifying lens. Sometimes, they’ll take digital photos of your retina. These images can be reviewed later or sent to specialists remotely. This isn’t a luxury. It’s your best defense.What’s Next? New Treatments on the Horizon
Laser therapy isn’t the only tool anymore. In recent years, injections of anti-VEGF drugs-like ranibizumab and aflibercept-have become common. These drugs block the signal that tells the eye to grow abnormal blood vessels. They’re especially effective for diabetic macular edema and often used before or after laser treatment. Some patients now get a combination: an injection to reduce swelling, then laser to prevent future growth. The goal isn’t to replace laser-it’s to use it smarter. Researchers are also testing longer-lasting medications and even implantable devices that slowly release drugs into the eye. AI-powered screening tools are being rolled out in clinics, helping catch early signs faster. But none of this matters if you don’t get checked.What You Can Do Today
You don’t need to wait for symptoms. You don’t need to be scared. You just need to act.- Get a dilated eye exam this year. If it’s been more than 12 months, schedule one now.
- Know your A1C. Aim for under 7%. If it’s higher, talk to your doctor about a plan.
- Control your blood pressure. Keep it under 130/80.
- Quit smoking. It’s not just bad for your lungs-it’s killing your eyes.
- Don’t ignore changes. Floaters? Blurry vision? Flashes of light? Call your eye doctor immediately.
Can diabetic retinopathy be reversed?
Early damage from diabetic retinopathy can be slowed or stopped with treatment, but once vision loss occurs-especially from scar tissue or detached retina-it usually can’t be fully reversed. That’s why early detection is critical. Laser treatment and injections can prevent further damage, but they don’t restore lost sight.
How often should I get my eyes checked if I have diabetes?
If you have type 1 or type 2 diabetes, you should have a dilated eye exam at least once a year. If you already have signs of retinopathy, your eye doctor may recommend exams every 3 to 6 months. Pregnant women with diabetes need an exam in the first trimester and possibly more during pregnancy, as hormonal changes can speed up retinopathy.
Does laser treatment hurt?
Most people feel pressure or mild discomfort during laser treatment, but not sharp pain. Numbing drops are used before the procedure. You might see bright flashes of light. Afterward, your vision may be blurry for a few hours, and you’ll need someone to drive you home. Some people notice a slight dimming in peripheral vision or trouble seeing in the dark afterward-that’s normal and part of how the treatment works.
Can I prevent diabetic retinopathy entirely?
You can’t guarantee you’ll never get it, but you can drastically lower your risk. Keep your blood sugar, blood pressure, and cholesterol under control. Don’t smoke. Get annual eye exams. Studies show people who manage their diabetes well have up to a 76% lower risk of retinopathy progression. Prevention isn’t about perfection-it’s about consistency.
Is laser treatment the only option for diabetic retinopathy?
No. For diabetic macular edema, injections of anti-VEGF drugs are often the first line of treatment. For proliferative retinopathy, laser is still standard, but sometimes used with injections. In advanced cases, surgery may be needed to remove blood or repair a detached retina. The best approach depends on the stage and type of damage-and it’s usually a combination of treatments, not just one.


13 Comments
Okay, but let’s be real-why is the FDA still letting Big Pharma push these $1,000-a-shot anti-VEGF drugs when laser treatment has been saving eyes since the 80s??!! We’re being sold a luxury fix while the real solution-blood sugar control-is treated like a suggestion!!!
you got this!! 🙌 i had diabetic retinopathy and got laser done-yes it was weird and bright but i can still see my grandkids’ faces. check your eyes. no excuses. you matter!!
They’re not warning you because they make more money off your blindness than your vision.
Wow. So the ‘95% preventable’ stat is just a marketing gimmick to guilt people into checking their eyes while insulin prices skyrocket? Classic. You really think people with minimum wage jobs can afford ‘annual dilated exams’? 😂
Let me guess-this whole post was written by an ophthalmologist who’s never had to choose between insulin and groceries. You’re telling me to ‘control my blood sugar’ like it’s a yoga routine. Meanwhile, my food stamps only cover white bread and soda. Thanks for the guilt trip, Dr. Privilege.
America’s healthcare system is a joke. We’re told to ‘get screened’ but the clinics won’t take Medicaid. They want you to pay out of pocket for a test that should be free. This isn’t prevention-it’s exploitation. And don’t even get me started on how the VA ignores this in veterans.
Okay but I just got my annual eye exam and my doc said my retina looks AMAZING 😍 I’ve been hitting my A1C under 6.8 for 2 years now-IT’S POSSIBLE!! 🙏 You don’t need to be perfect, just consistent. And yes, laser sucks-but it’s better than losing your license. You got this, fam!! 💪✨
It is of the utmost importance to note that consistent glycemic control remains the cornerstone of retinopathy prevention. While laser photocoagulation remains efficacious, emerging therapies such as anti-VEGF injections offer enhanced outcomes in macular edema. One must not overlook the significance of biannual screenings for high-risk populations. Thank you for this well-researched article. 😊
As a nurse who’s seen 300+ diabetic patients over 15 years-I can tell you this: the ones who survive without vision loss? They’re not the ones with the best insurance. They’re the ones with someone reminding them to check their feet, take their meds, and show up for their eye appointments. It’s not magic. It’s love. And community. And showing up for each other. If you’re reading this and you’re scared-text your cousin. Call your sister. Don’t do this alone.
Interesting. But the study cited from Cleveland Clinic-was it prospective or retrospective? What was the sample size? Did they control for socioeconomic factors? And why is there no mention of the 2021 JAMA study showing anti-VEGF monotherapy outperforms laser in early DME?
my mom had this and got laser. she said it felt like someone was popping popcorn in her eye. weird, but worth it. she still drives. i got my exam last month. all good. thanks for the reminder.
Let me guess-this is all part of the ‘diabetes industrial complex.’ The real cause? Fluoride in the water. Glyphosate in your corn syrup. And the eye doctors? They’re paid by the FDA to scare you into treatments that don’t work. Your ‘95% preventable’ claim? Lies. They want you dependent on lasers and injections so they can keep billing Medicare. Wake up.
You speak of control as if diabetes is a moral failing. But in India, where I'm from, 70% of diabetics have no access to glucose meters. We eat rice because it’s cheap. We walk 10km to clinics. You talk of ‘annual exams’ like it’s a spa day. This isn’t about discipline-it’s about colonial healthcare systems that export our suffering as ‘lifestyle choices.’
Write a comment